888 CalPERS or 888-225-7377 TTY. Regional Offices are closed to in-person appointments due to COVID-19.
Pacific time seven days a week except state holidays.

State of california benefits phone number. Certify for benefits using EDD Tele-Cert SM. The Division works closely with the federal Centers for Medicare and Medicaid Services CMS so that the Department of Health Care Services can provide eligible Californians with access to affordable. The Golden State Stimulus aims to.
The Savings Plus Program provides additional opportunities to save for retirement with 401 k and 457 Plans. Copyright 2021 California Public Employees Retirement System CalPERS State of California. From employee pensions managed by the California Public Employees Retirement System CalPERS to health dental and vision plans state employment offers you many benefits.
Each phone number contains the corresponding information city state etc. Box 997421 MS 4719 Sacramento CA 95899-7421. In your UI Online account select Contact Us to request a change.
If you have general questions or need help with account registration password resets your EDD Account Number or how to use UI Online contact us at 1-800-300-5616 from 8 am. Health Insurance Premium Payment PO. 800 541-5555 outside of California please call 916 636-1980 Estate Recovery PO.
If you are a member or provider and would like to tell us about a problem with access to care please email us here. Email to get help with State services and programs or call 800-807-6755. Mail California Department of Social Services 744 P Street Sacramento CA 95814 Out-of-State Inquires cdssosidsscagov.
California CalWORKs TANF Administration for Children and Families ACF Living Assistance. These information is determined by the first six digits of the phone number. Sacramento CA 95899-7413 Not able to find answers to your questions.
Pacific time seven days a week except on California state holidays. Box 997417 MS 4607 Sacramento CA 95899-7417 916 552-9200. Request copies of your.
The program serves all 58 counties in the state and is. California will provide the Golden State Stimulus payment to families and individuals who qualify. California Secretary of State Contact Informations.
1 916-795-3000 Were closed on state holidays. To 5 pm Monday through Friday excluding state holidays To get help on questions related to the novel coronavirus COVID-19 please use the California Department of Public Healths Questions and Comments form. This is a one-time 600 or 1200 payment per tax return.
By Fax or Mail. Visit the California Department of Tax and Fee Administrations CDTFA website email the CDTFA find a local office or view their directory. Pacific time seven days a week except state holidays.
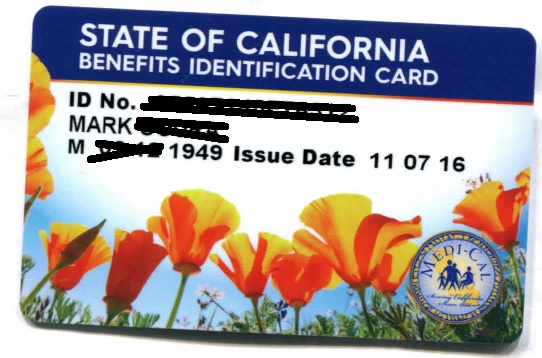
Frequently Used Phone Numbers. Pacific time Monday through Friday except on state holidays. Except State Holidays and CA only As a participant in the Medi-Cal program your feedback is important to us.
UI Automated Self-Service Line. Call the UI Customer Service line at 1-800-300-5616 available from 8 am. By clicking the number you can get more information about the number such as the zip code carrier etc.
English Self-Service Line Get information on your last payment issued. Customer service phone numbers. You can also certify for benefits using EDD Tele-Cert SM request copies of your 1099G tax information and find your local Americas Job Center of California SM.
Monday through Friday 8 am. Telephone 916 651-8848 Email piardsscagov. 800 959-6545 International Calls.
You may receive this payment if you receive the California Earned Income Tax Credit CalEITC or file with an Individual Taxpayer Identification Number ITIN. Get information on how to file a new claim or reopen an existing claim and your last payment issued. Get information on how to file a new UI claim or reopen an existing claim.
Box 997425 MS 4720 Sacramento CA 95899-7425 916 650-0490 Medi-Cal Eligibility PO. Child Care Assistance 800 543-7793 County Medical Services Program 800 670-6133 Lost or Stolen EBT Card 877 328-9677 Medi-Cal. California Department of Tax and Fee Administration PO Box 942879 Sacramento CA 94279-0001.
Technical Issues Using the CAgov Portal. We serve those who serve California. CalWORKs is a welfare program that gives cash aid and services to eligible needy California families.
Medi-Cal Benefits Division The Benefits Division is responsible for setting policy and covered services for health care services for the Medi-Cal program. You can also call 1-800-896-4042. EDD Customer Account Number.
You may be able to find the assistance you need on our list of contacts or call or email the Ombudsman. 1-877-238-4373 from 8 am.