76 lignes Drugs used for Birth Control The following list of medications are in some way related to or used in the treatment of this condition. While women can choose from bilateral tubal ligation in the hospital aka having your tubes.
 Which Birth Control Pill Is Right For Me Bedsider
Which Birth Control Pill Is Right For Me Bedsider
Permanent Birth Control.
Birth control list. Birth Control were from the start of their career tipped to be one of Germanys top rock acts. Androgenic Properties of Birth Control Pills How to choose the right birth control pill for you 35 mcgm Pill Brand Name Progestin Dose mg 50 mcgm Estrogen level ethinyl estradiol mg phasic 304030 mcgm phasic 3535 mcgm phasic 353535 mcgm 30 mcgm 20 mcgm. They also encourage the thickening.
Watch short videos about birthcontrol on TikTok. They were originally formed in late 68 by Bernd Koschmidder bass Reinhold Sobotta organ Rolf Gurra sax vocals and Egon Balder drums. What are birth control pills.
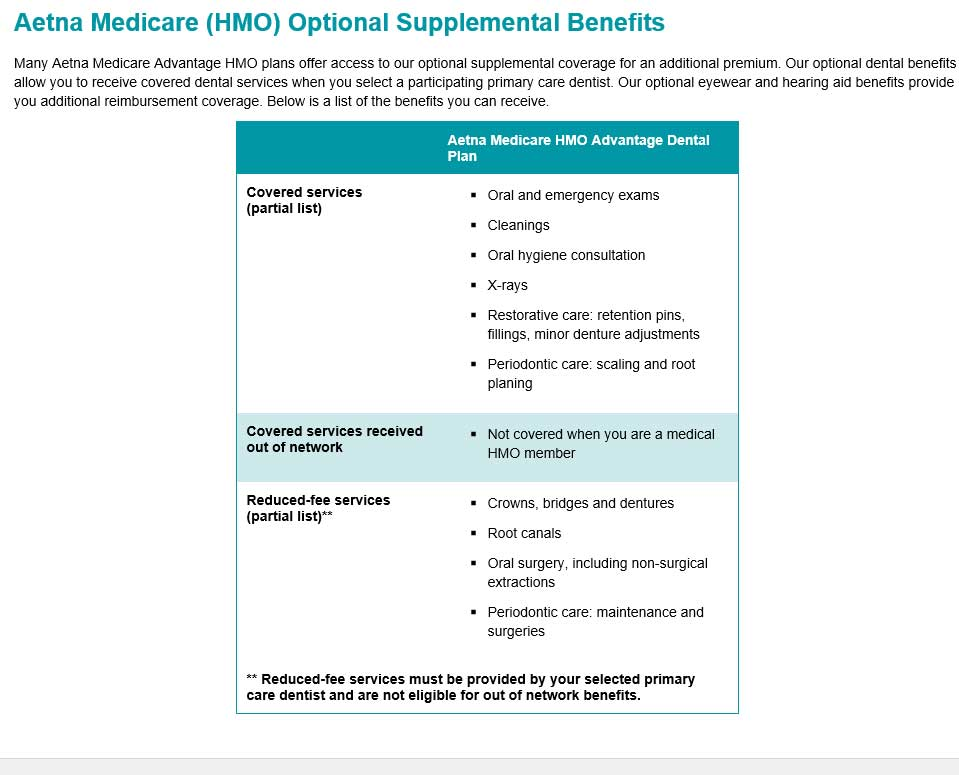
According to DailyMed triphasic birth control pills contain 21 days of active hormonal pills with different doses of estrogen and progestin each week. List of Birth Control Pills. Forms of birthContraceptive sponge control contraception are not currently considered Preventive Care Medications under the Affordable Care Act.
Types of Medicines and Devices for Birth Control. This includes both combination pills estrogen and progestin and the minipill progestin only. The fertile period starts 5 days before ovulation and continues for 3 days after.
Natural birth control methods include total and continuous abstinence and the rhythm method. Log in to follow creators like videos and view. Most birth control pills today are considered low-dose.
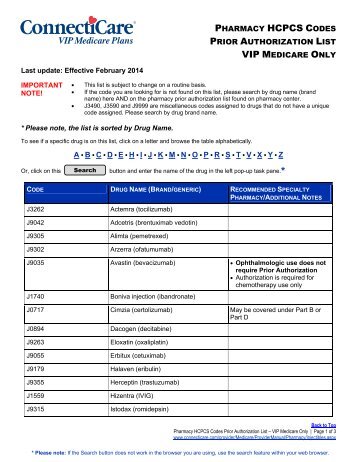
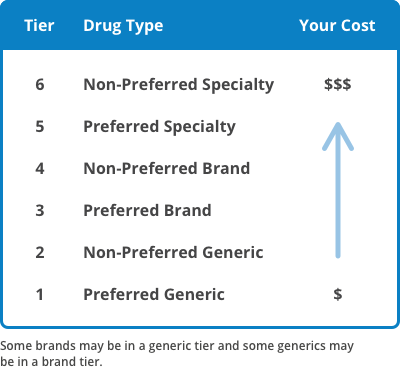
Low-dose pills contain 10 to 30 micrograms. Permanent birth control is not reversible and prevents pregnancy 99 of the time. Select drug class All drug classes hormonesantineoplastics 4 contraceptives 243 spermicides 3 progestins 30 sex hormone combinations 53 miscellaneous vaginal agents 4 progesterone receptor modulators 1.
A surgical procedure that makes a person who can produce sperm unable to cause a pregnancy or a person who can ovulate unable to become pregnant. But there are more types of birth control pills than ever before. A woman is fertile for 9 days every month during which she is most likely to conceive.
18 lignes This chart does not list all of the risks and side effects for each product. The Pill aka oral contraception may still be what many women think of first when we think of birth control. Egon left in 1969 and Bruno Frenzel guitars vocals and Bernd Noske drums vocals joined.
At this time we do not submit claims to insurance for the medical consult fee. With a lot of talk by Pope Paul about abolishing the pill and other forms of contraception they thought that the name Birth Control. This includes unlimited messaging with our medical team about your birth control for one year so you can request prescription changes or ask questions any time during that period.
Norethindrone Acetate EE. Birth control pills are oral contraceptives that contain hormones which prevent your ovaries from releasing eggs during ovulation. Talk to your healthcare provider about the best method for you.
Birth control 1B people have watched this. This page lists FDA-approved and cleared methods for birth control. Contraceptive foams Contraceptive gels s Emergency birth control contraceptives generic for Plan B generic for Plan B One-Step Femalecondoms.
The rhythm method involves having no intercourse or protected intercourse during the time when the woman is fertile. Birth Control Anyone who requests a birth control prescription will be charged a 15 consultation fee. 283 lignes Hormonal contraceptives are available as pills oral contraceptives injections.