Watch this video and click the link ab. Dental insurance policies with benefits for adult orthodontia may cover from 25 to 50of the costs.
Will Dental Insurance Cover Invisalign Plaza Dental
Delta Dental has a pretty good track record of covering braces and Invisalign compared to other insurers if your plan includes orthodontic benefits.

What dental plans cover orthodontics. Dental insurance that covers braces for adults Finding a dental insurance planthat includes coverage for. You might be covered for orthodontic services under your Delta Dental plan. The annual premium is 105 and your expense for 24 months of orthodontic treatment is 2500 which is about 50.
Dental insurance plans often have an annual maximum which is the maximum. With indemnity dental insurance you can visit any dentist there are no networks or approved providers. That means they cover preventive care at 100 basic procedures at 80 and major procedures at 50 or a larger co-payment.
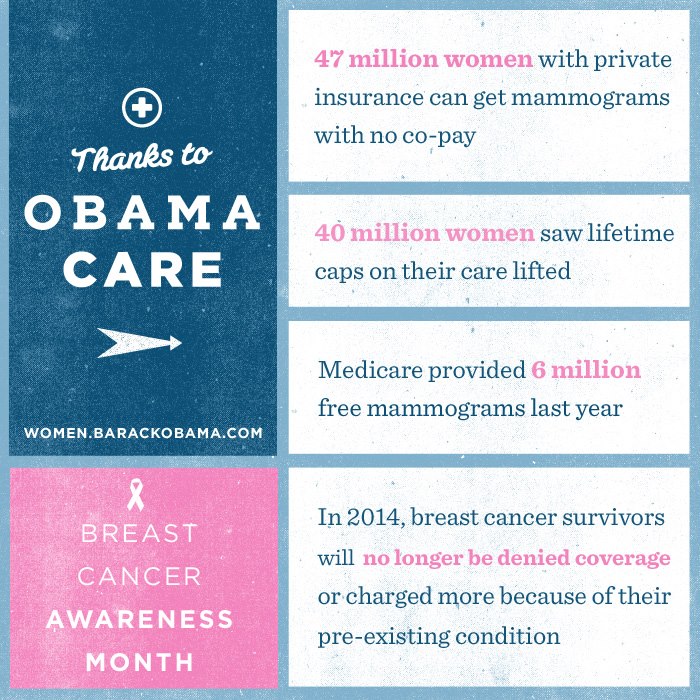
Pre-existing conditions are no problem. Most plans follow the 100-80-50 coverage structure. 1Your benefits may differ from the general information provided here.
To find out review your Contract Policy or Evidence of Coverage booklet or check with your benefits administrator. Our best dental insurance plans with no waiting period roundup reviews cost coverage. There is also a twelve-month waiting period and a lifetime limit of 1000.
Several factors can affect the cost of orthodontic care including the recommended type of treatment and whether you have dental insurance. Dental insurance is not an essential benefit so health insurance plans do not automatically cover dental and orthodontic care orthodontic health insurance is covered by a supplemental health plan which you will have to add on to your health insurance or purchase separately. Your orthodontic coverage and options may vary based on your plan type.
You pay a deductible on your indemnity dental insurance after which the insurance provider will cover a part - typically between 50 and 80 of reasonable and customary dental costs as well as 100 of your preventative care. Orthodontic care may not be covered if you begin treatment before you start a dental insurance plan. If you are considering braces check with your insurance provider to see if some or all of the cost will be assumed by the provider.
Dental savings plans sometimes known as dental discount plans are particularly well-suited to making orthodontics affordable. Savings vary based on plan members locations the average rate for dental care locally and the savings negotiated by plan providers. Depending on the plan you choose you may have a range of discounts on the cost of braces and other devices.
And you can get up to 50 covered which is right in line with most other providers. 7 Be sure to get dental coverage. On the other hand DeltaCare USA PAA48 is an example of an individual dental program that covers orthodontic treatment for adults.
Patients are responsible to pay the remaining charges. You have to pay 50 of the providers fee after meeting a lifetime deductible of 50. Orthodontics such as braces are not covered by most plans but it is possible to find a dental plan that covers braces.
Its also common for dental insurance plans that cover orthodontics to only provide coverage for children up to age 19. But a dental plan. If you discover that your current policy does not cover orthodontics you can supplement it with a more inclusive dental plan.
In some cases private individual and family plans offer dental insurance for orthodontic care. Dont put essential dental procedures on hold while you wait for insurance to kick in. Cigna Dental 1500the companys most comprehensive dental planoffers coverage for orthodontic work.
Employer-sponsored dental insurance plans sometimes contain this optional coverage. 1 If you are interested in orthodontic insurance or a good dental plan that will. 5 Many Humana dental insurance plans offer discounts on adult and child orthodontic care.