Call Covered CA at 1-800-300-1506. For Covered California Members LA Care Health Plan is allowed 45 working days from the day of receipt to finalize a claim.
Https Www Coveredca Com Medicare Attestation Form Pdf
Improving Access Affordability and Accountability.
Covered california status. The open-enrollment period for coverage during 2014 will run from Oct. Covered California only requires that the person seeking health coverage show proof of immigration status. You are already enrolled in a Covered California plan and become newly eligible or ineligible for tax credits or cost-sharing reductions.
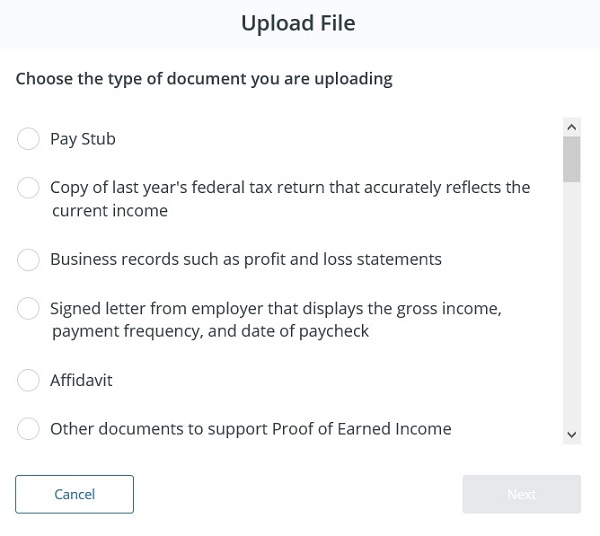
You can report your changes to Covered CA in one of the three ways below. Both lawfully present and not lawfully present individuals can apply through Covered California to see if they are eligible for a health plan through Covered California or Medi-Cal. Find out about Covered California enrollment on our Data and Research webpage.
Covered California Holding Health Plans Accountable for Quality and Delivery System Reform. One of the many things you want look out for is your account status in your online Covered California application account. The Employment Authorization Document I-766 annotated Category C33 is specific to DACA and is not proof of eligibility for Covered California.
Now lets look at this in practical terms. Each claim is subject to a comprehensive series of quality checks called edits and audits Quality checks verify and validate all claim information to determine if the claim should be paid denied or suspended for. Covered California is a free service from the state of California that connects Californians with brand-name health insurance under the Patient Protection and Affordable Care Act.
Covered Californias First Five Years. If you are eligible for Medi-Cal the open enrollment period does not matter. If you do your coverage wont begin on the effective date you originally signed up for.
A System Status Alert will be posted on the Medi-Cal website before the scheduled system upgrades. Covered California Comments on Web-Based Entities and Enhanced Direct Enrollment CMS-9934-P. Its the only place where you can get financial help when you buy health insurance.
The alert will provide additional details including the anticipated extended maintenance window time frame. Deferred Action for Childhood Arrivals DACA is not an eligible immigration status for health insurance through Covered California. Protecting Privacy Covered California uses the information provided on an individuals application.
1 2013 for coverage that will take effect Jan. Contact Covered CA to report your changes if no members in your household have Medi-Cal. Covered California Options To Improve Affordability.
Covered California will begin enrollment on Oct. You are already enrolled in a Covered California plan and you lose a dependent or lose your status as a dependent due to divorce legal separation dissolution of domestic partnership or death. Individuals granted Deferred Action Status Notice of Action I-797 showing approval of deferred action status.
It depends on how your household is enrolled. Information on Cost-Sharing and Payments With Respect To Out-of-Network Coverage. 1 2013 to March 31 2014.
Employment Authorization Document Card I-766 annotated C14. Enrollee Rights Information Under Title I of the Affordable Care Act. Coverage through Covered California either a Covered California Health Plan or Medi-Cal will be asked for information to verify their citizenship or lawfully present status such as a Social Security Number or Alien Number.
Interest is due on a late paid claim. There is no waiting period or five-year bar. Providers who subscribe to the Medi-Cal Subscription Service MCSS and select the System Status Alert option will receive an email notification when an alert is posted.
Non-immigrant status holders including worker visas and student visas. If you have a status of pending you DO NOT want to make changes to your account. Family members who are not applying for medical coverage will not be asked for their proof of lawful presence.
Any documents and information provided by individuals applying for coverage through Covered California will not be used for any purpose other than to. Covered California Comments on Small Business Health Options Program CMS-9934-P Covered California Comments on Standardized Options and Differential Display CMS-9934-P Covered California Comments on User Fee CMS-9934-P - Updated.