The list below includes specific equipment services drugs and procedures requiring review andor supplemental documentation prior to payment authorization. Prior Authorization A process that allows physicians and other professional providers to determine before treating a patient if Blue Cross Blue Shield of Michigan will cover the cost of a proposed service.
Https Www Bcbsil Com Pdf Education Forms Fhp Preauth Form Pdf
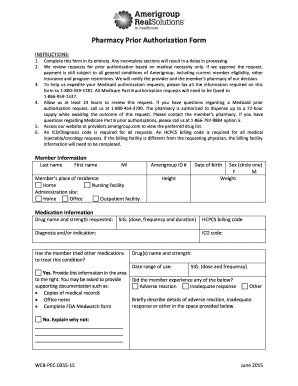
Medical policy precertification and preauthorization router.

Bcbs prior authorization list. Advanced Imaging - Prior Authorization. Inpatient services and nonparticipating providers always require prior authorization. For BCN commercial members effective Aug.
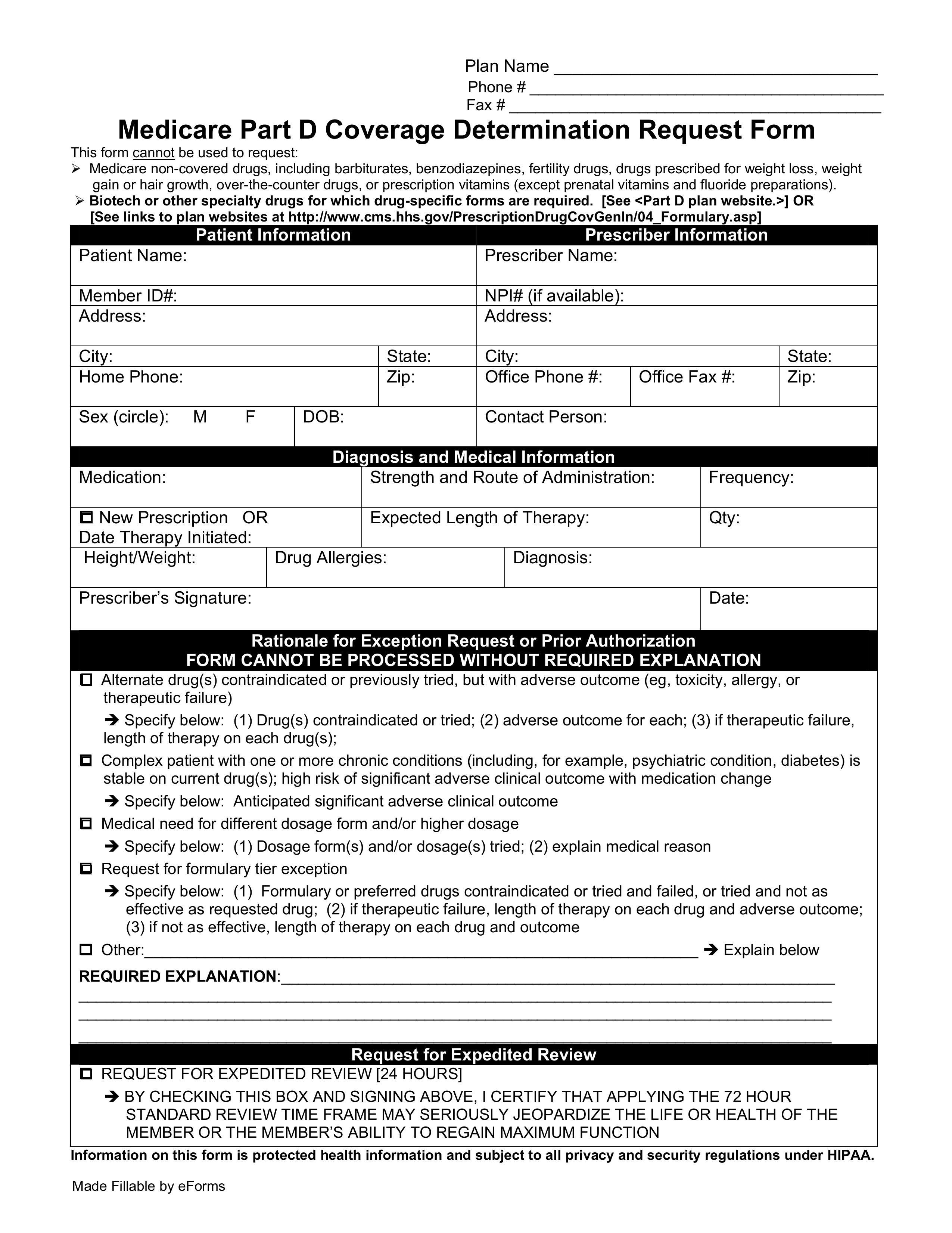
Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity as defined by the members health benefit plan. The following list is a guide to the types of genetic and genomic tests that require precertification. Urgentemergency admissions do not require prior authorization.
For dates of service on or after Jan. Precertification is required for many services including the following outpatient hospital benefits physician benefits and other covered services. 1 2019 You must submit authorization requests prior to administering any of the drugs on this list for those drugs to be eligible for payment.
List of services requiring authorization. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review. BCBSM requires prior authorization for services or procedures that may be experimental not always medically necessary or over utilized.
These lists are not exhaustive. Due to the volume of tests it is not possible to list each test separately. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Do not require prior authorization. Once youve checked member benefits and eligibility our Outpatient Surgical Day Care List can help you in making level of care determinations. 15832 EXCISE EXCESSIVE SKIN THIGH Pre-operative evaluation history and physical including.
Rendering BCBSRI Policy Implantable Cardioverter Defibrillator. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. Some services require prior authorization preauthorization before they are performed.
The procedures or services on the lists below may require prior authorization or prenotification by BCBSTX Medical Management or other designated vendor for certain designated groups. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. This list will be updated no more than twice a calendar year.
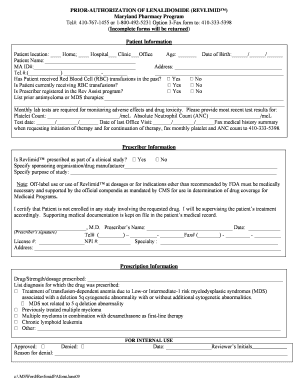
Obtaining a prior authorization helps us pay claims faster with no denied charges or unexpected costs to our members. Prior Authorizations Lists for Designated Groups. The approval criteria were developed and endorsed by the Pharmacy and Therapeutics Committee and are based on information.
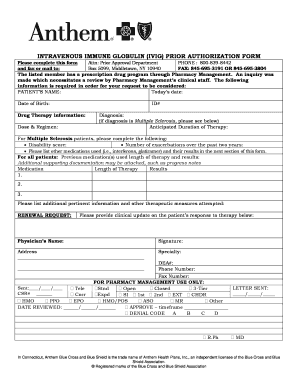
1 2021 TurningPoint Healthcare Solutions LLC manages authorization requests. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. The Prior authorization list is a list of designated medical and surgical services and select prescription Drugs that require prior authorization under the medical benefit.
Radiological services such as CT CTAs MRIsMRAs PET scans and nuclear medicine and cardiovascular system procedures myocardial imaging myocardial infusion studies and cardiac blood pool imaging. For members who have prescription drug coverage through Independence Blue Cross Independence prior authorization is required for certain prescribed formulary drugs in order for such drugs to be covered. The presence of codes on these lists does not necessarily indicate coverage under.
Below is the list of specific services in these categories that require precertification. Procedures Tests Services Requiring Preauthorization CPTHCPCS codes Preauthorization Method Responsible Provider. Require Prior Authorization Description of Procedure Code Medical Records Request Information Required 15830 EXC SKIN ABD Pre-operative evaluation history and physical including functional impairment and operative report.
Outpatient Surgical Day Care List January 2020. A prior authorization is not a guarantee of. Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts.
This tool does not reflect benefits coverage nor does it include an exhaustive listing of all noncovered services in other words experimental procedures cosmetic surgery etc refer to your provider manual for coveragelimitations. Update to Prior Authorizations Jan1 2021 Whats New. You may be responsible to pay for the services that are not approved.
The following documents pertain to procedures for which the Medicare Plus Blue Utilization Management department manages authorizations for dates of service prior to Jan. To determine if a test requires precertification please see the complete procedure code list for details. 1 2021 Blue Cross and Blue Shield of Texas BCBSTX will update its list of Current Procedural Terminology CPT codes requiring prior authorization to comply with changes as a result of new replaced or removed codes implemented by the American Medical Association AMA and BCBSTX Utilization Management updates.
Medical oncology prior authorization list for UAW Retiree Medical Benefits Trust PPO non-Medicare members. If you are performing a procedure on this list in an outpatient setting no prior authorization is required unless required by medical policy.