Unfortunately though Medicare does not cover medical alert systems. As a UnitedHealthcare Medicare Advantage member you are eligible to receive the Philips Lifeline medical alert service at no cost to you.
 Does Medicare Cover The Cost Of Medical Alert Systems 2021
Does Medicare Cover The Cost Of Medical Alert Systems 2021
Nursing home help assisted living subsidized senior housing or housing supportive services.

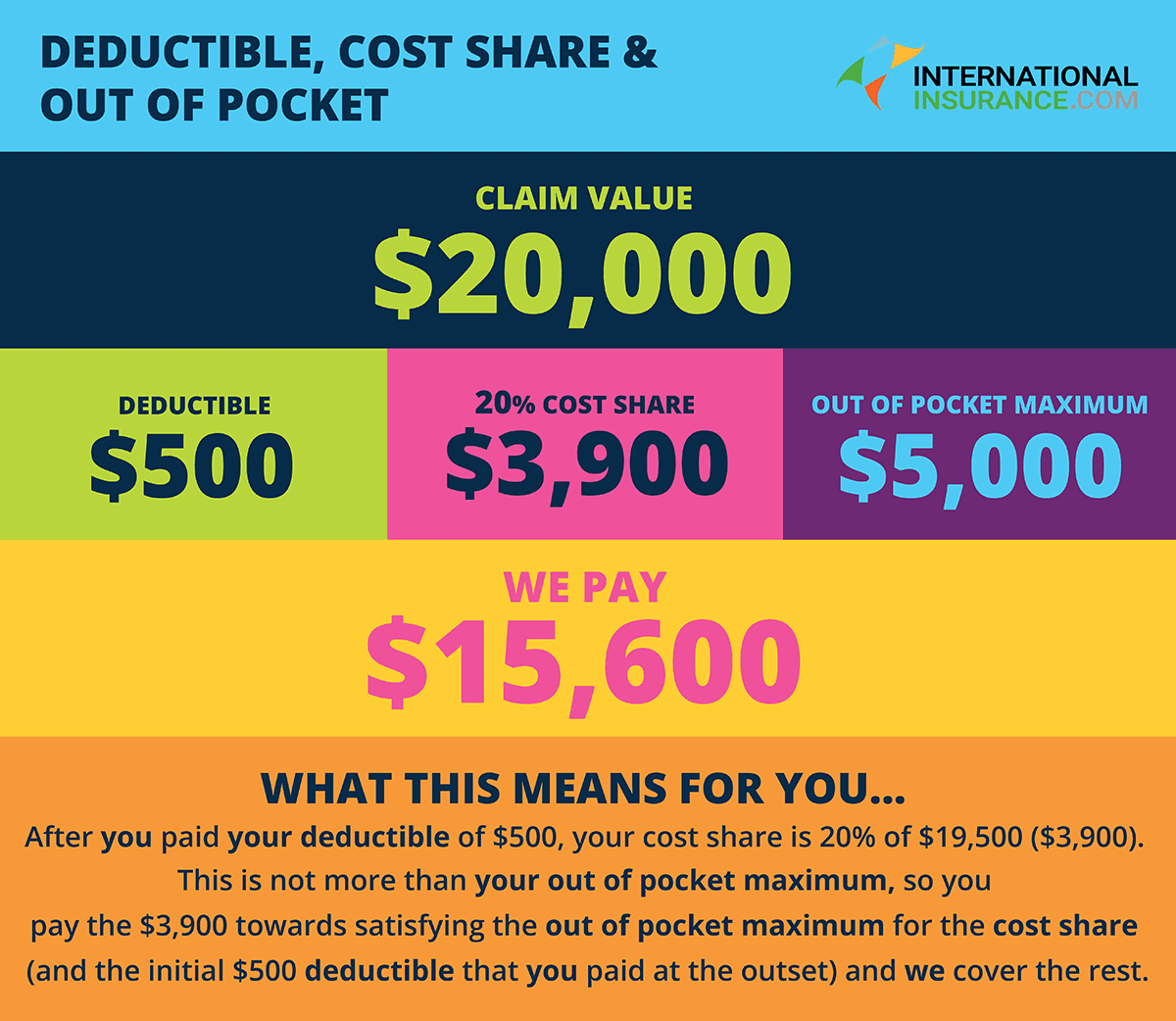
Does medicare pay for life alert. Medicare wont pay for medical alert systems but Medicare Advantage or Medicaid may help pay for some or all of the costs. What Medicare Coverage Options are Available for Life Alert. Does medicare pay for life alert You can pay your Medicare Part A Medicare Part B and Medicare Part D income-related monthly adjustment amount IRMAA online using MyMedicareMedicare also accepts payments from your banks online bill pay serviceMany Medicare Advantage Medicare Part D and Medigap plans accept online.
Several housing options are. Dependability is key to peace of mind. You may be wondering if Medicare covers medical alert systems.
The best way to see if this discount is available is to call your carrier representative and ask. But again youre not just paying for a medical alert system youre paying to receive around-the-clock emergency coverage from a pioneer in the medical alert industry. Medical Care Alert is another company that offers an affordable in-home system for low-income seniors.
If you are enrolled in Medicare Part A and Part B Original Medicare and want to obtain Life Alert or another. Contacting a device company directly to ask about discounts can. Medicare coverage is often only provided for services or supplies that are deemed to be medically necessary.
Find affordable quality Medicare insurance plans that meet your needs. Medicare Advantage plans might offer coverage for Life Alert. Life Alert Base Station.
Unfortunately Medicare Part B generally doesnt cover medical alert systems. Original Medicare does not cover Life Alert costs or the costs of other similar emergency medical alert systemsEmergency medical alert systems are designed specifically to help seniors living alone to remain independent and feel safe doing so. Although Original Medicare doesnt cover Life Alert some Medicare Advantage plans also called Medicare Part C may cover Life Alert medical alert systems and other personal emergency response system PERS systems as an added benefit.
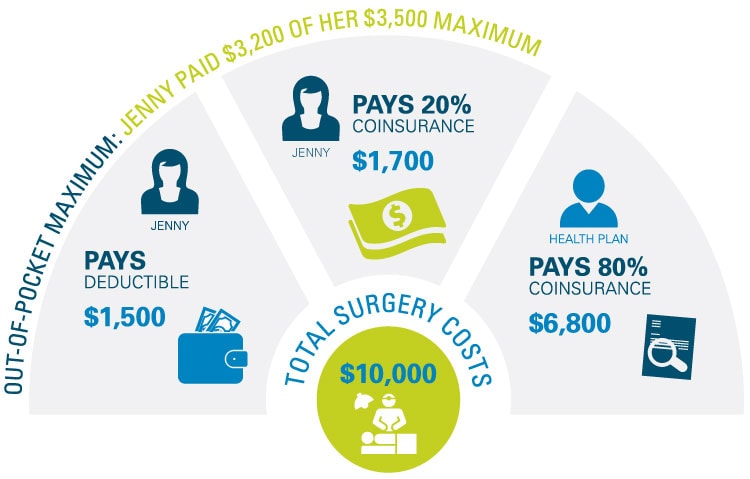
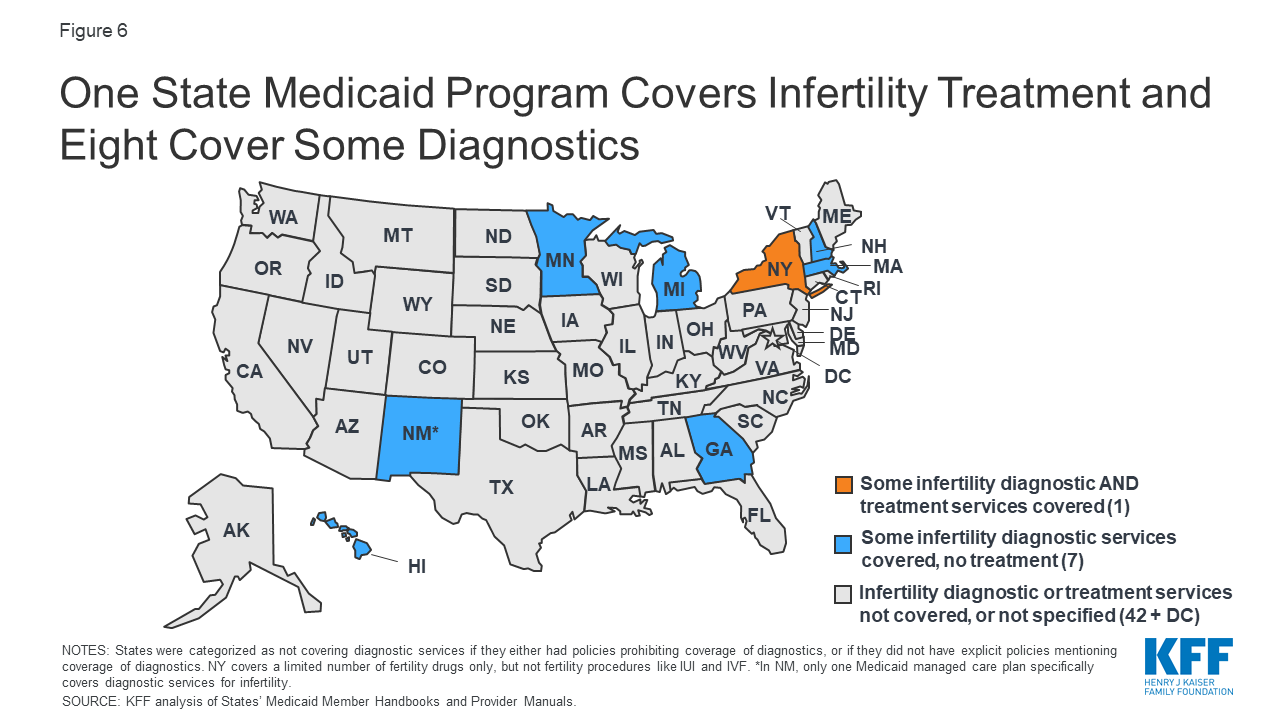
Find affordable quality Medicare insurance plans that meet your needs. Some Medicare Advantage Plans Medicare Part C cover medical alerts but this will vary with the insurance youre carrying and the state in which you live. Part B of Original Medicare covers durable medical equipment such as hospital beds canes walkers and blood sugar meters1 By that definition you might expect Medicare to cover medical alert systems.
But some Medicare health plans such as certain Medicare Advantage plans might cover them. In most cases Original Medicare plans do not provide coverage for medical alert systems. Since Medicare part A and B do not pay for Life Alert response systems or other emergency response services elderly patients may need to check other options available for the coverage.
Anzeige Shop Medicare plans from Aetna Humana UnitedHealthcare Wellcare Cigna Kaiser more. Original Medicare Part A and Part B typically does not cover medical alert systems. When compared to Medical Guardian and other great brands we found that Life Alert is sometimes twice as expensive.
Anzeige Shop Medicare plans from Aetna Humana UnitedHealthcare Wellcare Cigna Kaiser more. If seniors need more coverage to improve the quality of their life the ability to lead an independent life and flexibility they can sign up for a suitable Medicare Advantage Plan offered by a. Still that shouldnt stop you from getting a system.
Unfortunately Original Medicare doesnt cover medical alert systems. The cost to you will depend on your Advantage plan and the Life Alert coverage options you. Additionally senior military retirees who enroll in Tricare For Life and opt for a Medicare Part C plan may be able to obtain coverage for a medical alert system through a private provider.
Medicare Advantage plans may provide medical alert emergency response systems for. Original Medicare doesnt cover Life Alert. Most people are paying cash for medical alerts out of pocket.
Some Medicare Supplement insurance carriers may provide a discount on the cost of a medical alert system. Does medicare pay for life alert buttons If you are a senior citizen who is faced with mounting housing payments maintenance and medical costs Medicare offers housing assistance options. 45 years ago we founded the medical alert service industry and are still the 1 medical alert service in the US.
However if you receive your Part A and Part B benefits through a Medicare Advantage plan you can ask your plan if it covers these systems. If you have a Medicare Advantage plan check with your provider to see if they pay for medical alert systems.