Advertentie Unlimited access to Dental Insurance market reports on 180 countries. Other plans may require a 12 month waiting period.
 Dental Implant Insurance Coverage Plans No Waiting Periods
Dental Implant Insurance Coverage Plans No Waiting Periods
Waiting out a waiting period.
Dental insurance no waiting period for basic services. No Waiting Periods for Preventative Basic or Major Services - Use any Dentist or PPO Provider Annual Maximums of 1200 to 5000 per Person - Includes three cleanings and two exams per calendar year paid 100 Major Services are Paid 50 in CT and IL Starting Day One. Preventative dental procedures often do not have a waiting period while various basic procedures come with a minimum 3-month waiting period and you may have to wait anywhere from 6-12 months before you get coverage for any of the major procedures. Waiting periods differ from plan to plan but there is typically no waiting period for preventive or diagnostic services such as routine cleanings and basic exams.
However if you select a plan with Orthodontia services you may find depending upon your state of residence a waiting period on this service. A typical waiting period for major services could be anywhere from 12 to 24 months. Both plans increase Delta Dentals cost-sharing of out-of-pocket expenses after the first and second years of maintaining the policy.
The catch is that the premiums are usually higher. As you review no waiting period dental plans read the plan information to understand what the waiting periods look like and what coverage exclusions are part of the plan. Dental insurance plans with no waiting period for major dental work are extremely advantageous over those with a yearlong waiting period if you are in urgent need of major work.
In PA waiting periods do not apply to covered basic dental care services. In NM a 6-month waiting period applies to covered major dental care services. Patients who receive rapid dental care can return to their daily responsibilities without worrying about a tooth causing them more physical pain embarrassment or long-term bone loss from the result of missing.
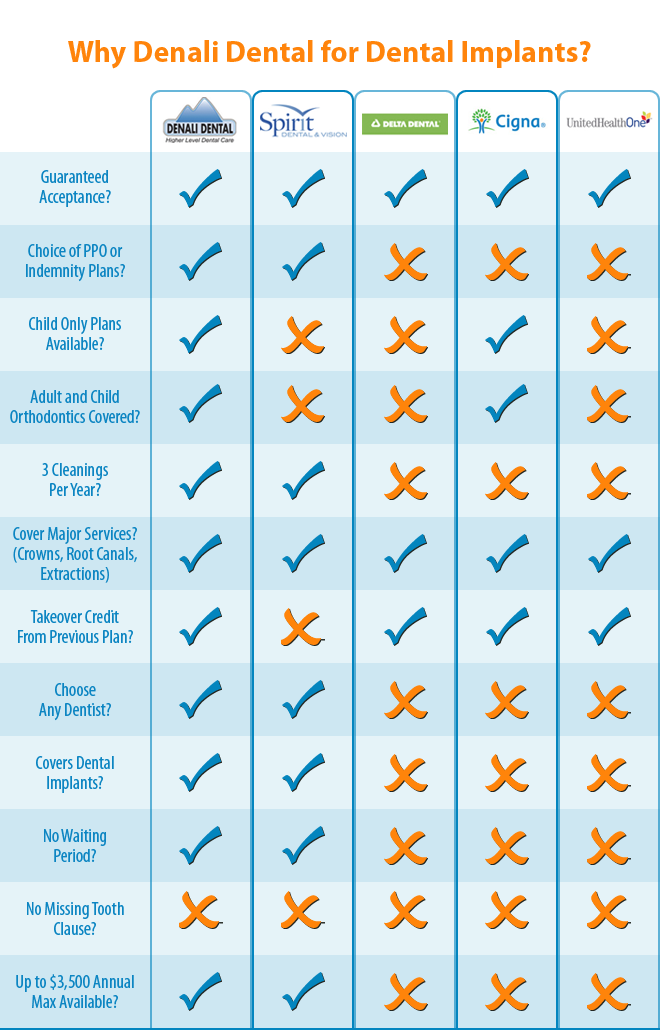
Waiting periods do not apply in RI. There are no waiting periods for Preventive Basic or Major services on the Spirit Dental plans. Download Reports from 10000 trusted sources with ReportLinker.
Conversely your dental plan may have a 6- to 12-month waiting period for restorative services such as filings and non-surgical extractions where a 12-month waiting period is often standard for major services such as crowns or dentures. If you dont need to undergo major dental work there are companies that offer full coverage dental insurance with no waiting for preventive and basic services to save on monthly premiums. In Arizona for example Delta Dental offers two plans with no waiting periods for basic and major services.
Delta Dental is a plan that will cover 100 of the Type I services in its insurance plan. 4 rijen Humanas three other dental insurance plans have no waiting period for preventive. Luckily there are some plans that do not have waiting periods for these restorative services.
Full coverage dental insurance with no waiting period means that you would encounter no waiting period for an array of services including major dental procedures. Many dental insurance plans have waiting periods for non-preventive care. For some companies there is no waiting period for major dental care.
Deltas plans are designed in a way that they offer no waiting period for services such Type I diagnosis and other preventive services which include x-ray tests dental examinations mouth cleanings and many more. Though policies vary greatly from provider to provider many dental insurance plans require a waiting period of anywhere from six to 12 months before theyll pay out any benefits for basic services. Across the US however the Humana Dental Loyalty Plus Plan has no waiting period ever.
Turquoise Plan and Copper Plan. The plans generally vary by state in some of which there is no required waiting period regardless of the procedure whereas others do have a six-month wait for fillings and basic oral surgeries. Luckily dental insurance with no waiting period takes the wait out of the equation.
In IL NJ and VT a 6-month waiting period applies to covered major and orthodontic dental care services. Download Reports from 10000 trusted sources with ReportLinker. Advertentie Unlimited access to Dental Insurance market reports on 180 countries.
All other states are paid at 25 Year One and 50 Year Two.