The Precertification Lookup Tool will let you know if clinical edits apply. Outside Los Angeles County.
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
To determine coverage of a particular service or procedure for a specific member.
Anthem blue cross prior authorization list. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Effective June 1 2020 prior authorization PA requirements will change for the following services to be covered for Anthem Blue Cross and Blue Shield members. Georgia Local PrecertificationPrior Authorization List Updated.
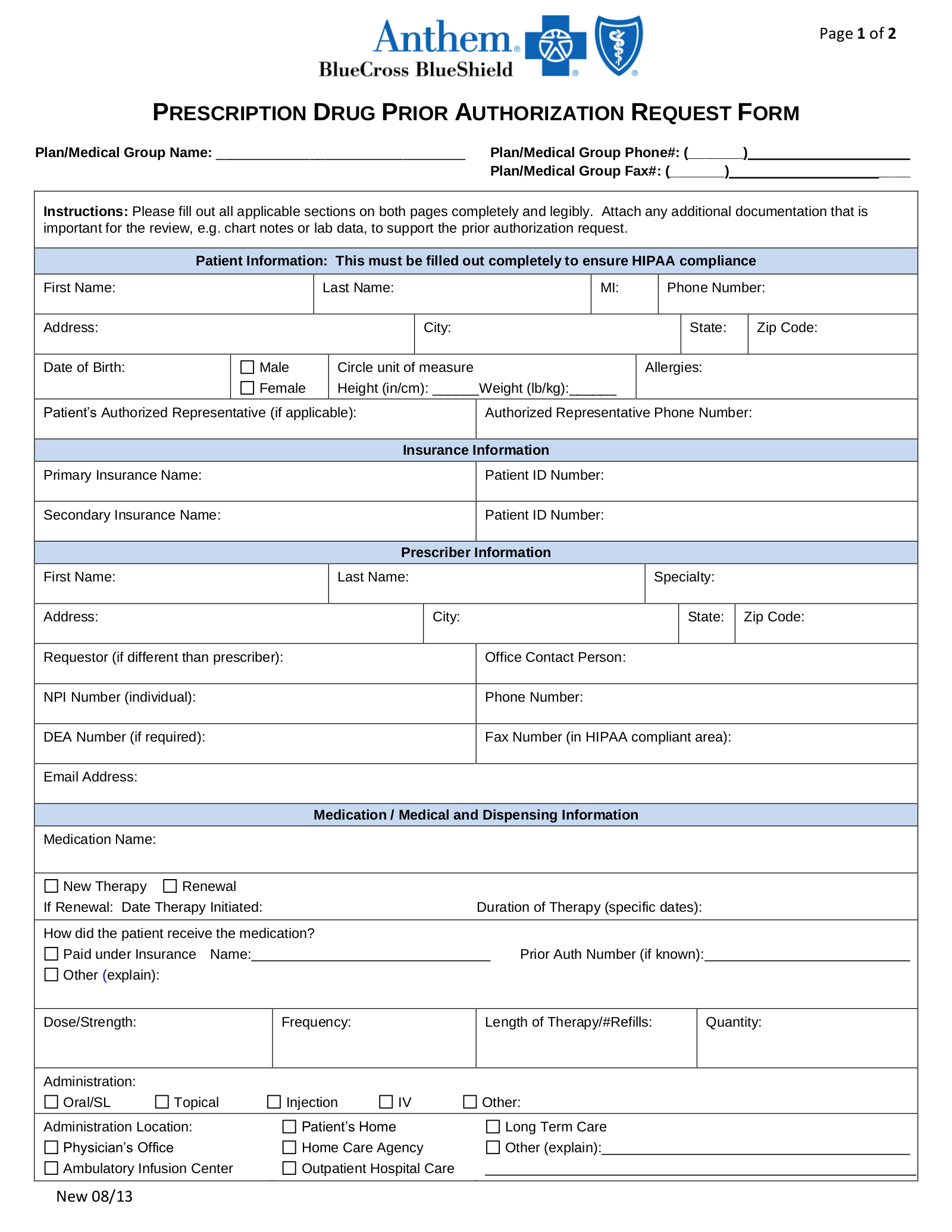
The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. For members who have prescription drug coverage through Independence Blue Cross Independence prior authorization is required for certain prescribed formulary drugs in order for such drugs to be covered. The services below require preauthorization.
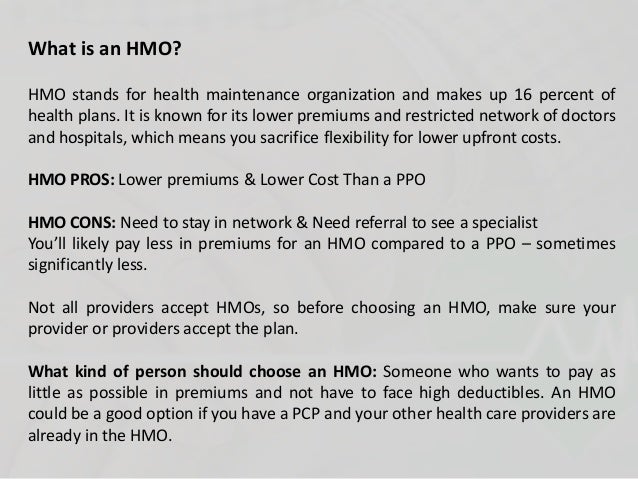
Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Customer Care Center hours are Monday to Friday 7 am. Hip Anthem ANC00009 15835 Excision excessive skin and subcutaneous tissue includes lipectomy.
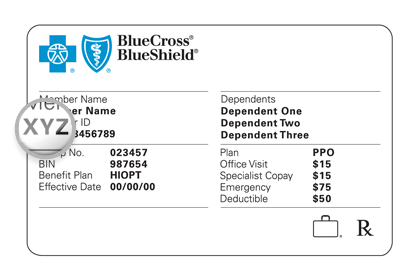
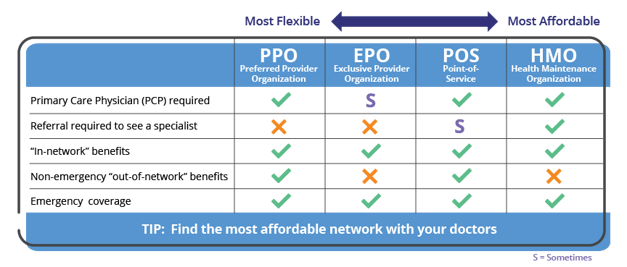
Your doctor can submit prior approval electronically by fax or by mail. Your doctor prescribes it in a medically appropriate way. Prior Authorizations Lists for Blue Cross Medicare Advantage PPO SM and Blue Cross Medicare Advantage HMO SM.
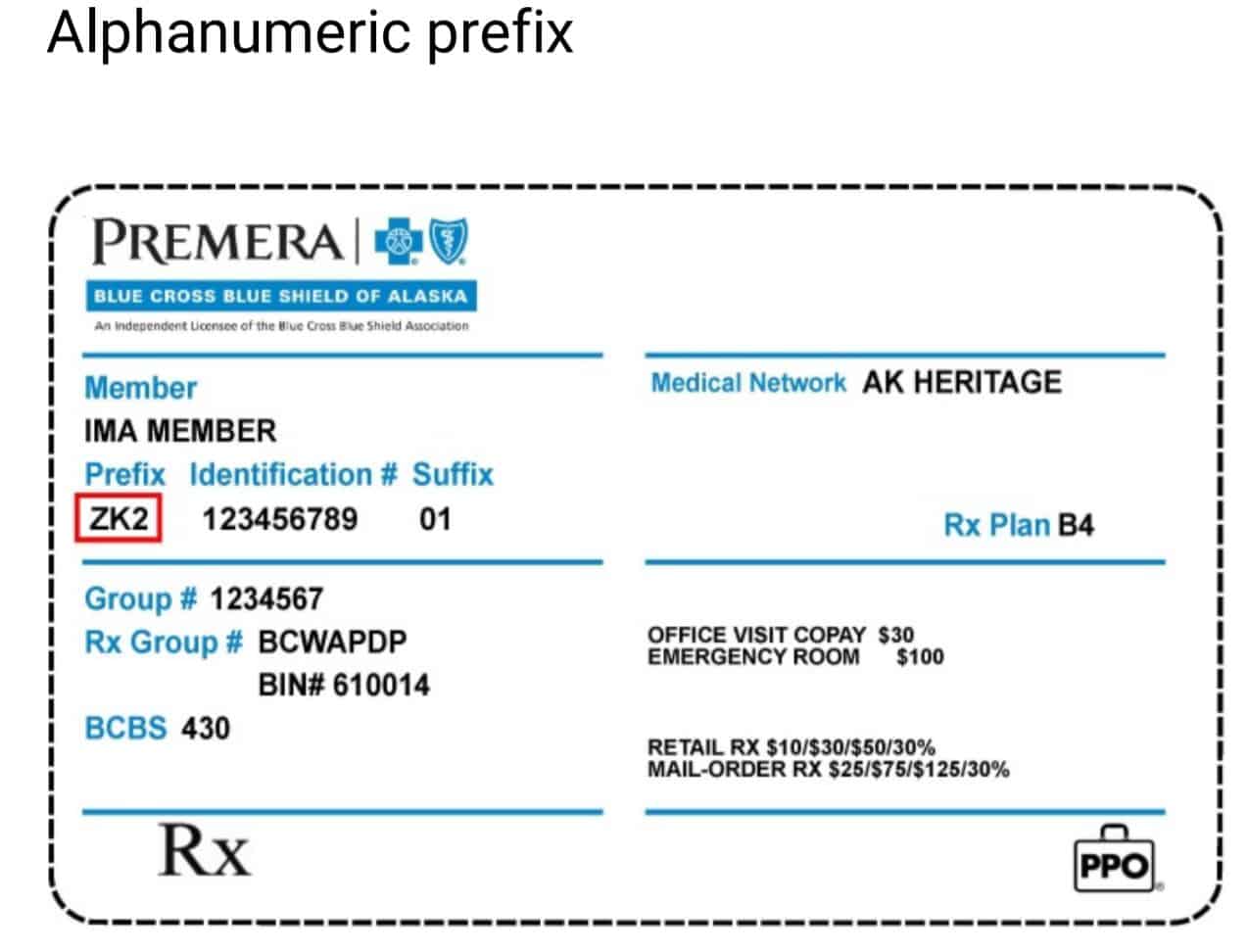
The Medicare Plus Blue prior authorization codes list PDF represents procedures that require authorization by eviCore healthcare for Medicare Plus Blue PPO members who reside in Michigan and receive services from Michigan providers. The approval criteria were developed and endorsed by the Pharmacy and Therapeutics Committee and are based on information. Use the Prior Authorization Lookup Tool within Availity or.
Radiological services such as CT CTAs MRIsMRAs PET scans and nuclear medicine and cardiovascular system procedures myocardial imaging myocardial infusion studies and cardiac blood pool imaging. These lists are not exhaustive. Advanced Imaging - Prior Authorization.
Forms and additional information can be downloaded on the CVS Caremark website. Buttock Anthem ANC00009 15836 Excision excessive skin and subcutaneous tissue includes lipectomy. Notice of Material ChangesAmendments to Contract and Changes to Prior Authorization Requirements may apply for new or updated reimbursement policies medical policies or prior authorization requirements.
Anthem Blue Cross and Blue Shield Healthcare Solutions Anthem has an online tool that displays prior authorization guidelines to help you quickly determine whether certain services for Anthem members require a prior authorization. Below is a list of some of the most common services requiring preauthorization or notification. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Anthem Blue Cross and Blue Shield Healthcare Solutions Medicaid Managed Care Pharmacy Prior Authorization Form Page 3 of 4 Describe medical necessity for nonpreferred medications or for prescribing outside of FDA labeling. You can access the Precertification Lookup Tool through the Availity Portal. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required.
Inside Los Angeles County. Access eligibility and benefits information on the Availity Web Portal or. The procedures or services on the below lists may require prior authorization or prenotification by BCBSTX Medical Management eviCore Healthcare or Magellan Healthcare.
010120 15834 Excision excessive skin and subcutaneous tissue includes lipectomy. Inpatient acute medical facility admissions. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Services obtained outside the local participating provider network. To determine coverage of a particular service or procedure for a specific member. The Prior authorization list is a list of designated medical and surgical services and select prescription Drugs that require prior authorization under the medical benefit.
Anthem Blue Cross Anthem is available by fax or Interactive Care Reviewer ICR 247 to accept prior authorization requests. You can see the full list of prescription drugs that need to be approved on the CVS Caremark website. The table below outlines the services that require Prior Authorization PA for Anthem Blue Cross Medicaid Business members enrolled in Medi-Cal Managed Care Healthy Families Program HMO and EPO Access for Infants and Mothers AIM Program HMO and EPO and Major Risk Medical Insurance.
The list below includes specific equipment services drugs and procedures requiring review andor supplemental documentation prior to payment authorization. Providers must obtain authorization from eviCore before these services are provided. Federal and state law as well as state contract language and Centers for Medicare Medicaid Services guidelines including definitions and specific contract.
Acute rehabilitation facility admissions. Use the Prior Authorization tool within Availity or. _____ _____ _____ List.
Skilled nursing facility admissions. Call Provider Services at 1-800-450-8753 TTY 711 After hours verify member eligibility by calling the 247 NurseLine at 1-800-300-8181. May 2021 Anthem Provider News - Ohio.
Our Interactive Care Reviewer ICR tool via Availity is the preferred method for submitting prior authorization requests offering a streamlined and efficient experience for providers requesting inpatient and outpatient medical or behavioral health services for our members.