Against exoerythrocytic forms of the parasites. This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered.
 Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
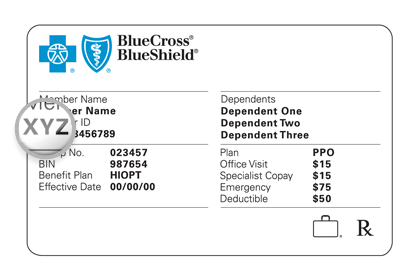
This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered.
Cvs caremark prior auth form. Insurance policies have their limitations and in some cases a physician must complete and submit the SilverScript prior authorization form in order to get approval for the drug they intend to prescribe to their patient. This patients benefitplan requires prior authorization for certain. Please respond below and fax this form to CVS Caremark toll-free at 1-866-249-6155.
Start a free trial now to save yourself time and money. This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered. Send completed form to.
The below form must be completed in its entirety by the medical practitioner prescribing the drug. Fax signed forms to CVSCaremark at 1-888-487-9257. Send completed form to.
CVS Caremark Prior Authorization 1300 E. Family of health care plans CVS caremark Osteoarthritis Prior Authorization Request Send completed form to. 1-855-330-1720 CVS Caremark administers the prescription benefit plan for the patient identified.
Send completed form to. Medicaid PA Request Form. CVSCaremark Prior Authorization Form California Created Date.
This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered. This patients benefit plan requires prior authorization for. Please respond below and fax this form to CVS Caremark toll-free at 1-866-249-6155.
1-866-249-6155 CVSCaremark administers theprescription benefit plan for the patient identified. CVS Caremark Criteria Type. CVS Caremark has made submitting PAs easier and more convenient.
Prior Authorization Request. To make an appropriate determination providing the most accurate diagnosis for the use of the prescribed medication is necessary. CVS Caremark administers the prescription benefit plan for the patient identified.
Prior Authorization Request. CVSCaremark Prior Rx Authorization Form The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription. Prior Authorization Request.
CVS Caremark administers the prescription benefit plan for the member identified. Pharmaceutical manufacturers not affiliated with CVS Caremark. Campbell Road Richardson TX 75081 Phone.
Medicaid PA Request Form. Formulary ExceptionPrior Authorization Request Form Patient Information Prescriber Information Patient Name. To make an appropriate determination providing the most accurate diagnosis for the use of the prescribed medication is necessary.
Fill out securely sign print or email your cvs prior form instantly with SignNow. Some automated decisions may be communicated in less than 6 seconds. CVS Caremark administers the prescription benefit plan for the patient identified.
CoverMyMeds automates the prior authorization PA process making it the fastest and easiest way to. A SilverScript prior authorization form is required in order for certain drug prescriptions to be covered by an insurance plan. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark.
Case Review Unit CVS Caremark Specialty Programs Fax. Weve partnered with CoverMyMeds and Surescripts making it easy for you to access electronic prior authorization ePA via the ePA vendor of your choice. Select the appropriate CVS Caremark form to get started.
Brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Caremark. Case Review Unit CVS Caremark Prior Authorization Fax. Contact CVS Caremark Prior Authorization Department Medicare Part D.
Prior Authorization Form Internal Use Only UMWA FUNDS Preferred Product Program Exceptions UMWA Funds This fax machine is located in a secure location as required by HIPAA regulations. This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered. Cvs Caremark Prior Auth Form.
If you wish to request a Medicare Part Determination Prior Authorization or Exception request please see your plans website for the appropriate form and instructions on how to submit your request. Send completed form to. 1 QUANTITY LIMIT PRIOR AUTHORIZATION CRITERIA BRAND NAME generic chloroquine hydroxychloroquine Status.
Case Review Unit CVS Caremark Prior Authorization Fax. Case Review Unit CVS Caremark Prior Authorization Fax. The most secure digital platform to get legally binding electronically signed documents in just a few seconds.
Available for PC iOS and Android. Case Review Unit CVS Caremark Prior Authorization Fax. CoverMyMeds is CVS Caremark Prior Authorization Formss Preferred Method for Receiving ePA Requests.
The CVS Caremark Prior Authorization Request Form can be used to request coverage for a non-formulary medication or one which is more expensive than those which are typically covered by the insurance company. Post Limit Prior Authorization POLICY FDA-APPROVED INDICATIONS. Completereview information sign and date.