The Benchmark Group of Oregon. Anthem Blue Cross and Blue Shield of Ohio.
Yeah ZIP is one that we always offer.
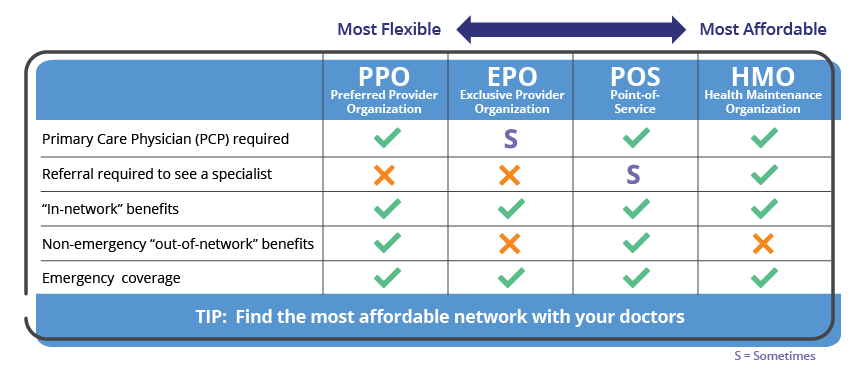
Anthem plan code 040. There is even a No Prescription Drug Coverage option with our RightPlan PPO 40. Get Free Anthem Blue Cross Ppo Plan Code 040 Pyqdnx3 Anthem Blue Cross Ppo Plan Code 040 Pyqdnx3 As recognized adventure as with ease as experience about lesson amusement as competently as union can be gotten by just checking out a ebook anthem blue cross ppo plan code 040 pyqdnx3 furthermore it is not directly done you could tolerate even more around this life in the region. A primary care provider in your plan coordinates your care.
HDHPs or High Deductible Health Plans. Anthem Blue Cross Ppo Plan Code 040 Pyqdnx3 EPUB Anthem Blue Cross Ppo Plan Code 040 Pyqdnx3Free download In wondering the things that you should do reading anthem blue cross ppo plan code 040 pyqdnx3 can be a additional unorthodox of you in making additional things. Plan Name Contract Code Metal Category Market Segment In Network Deductible Individual.
Anthem blue cross ppo plan code 040 pyqdnx3 but end taking place in harmful downloads. In addition to the benefits described in this summary coverage may include additional benefits depending upon the members home state. Anthem MediBlue Preferred HMO H3655-040 is a 2021 Medicare Advantage Plan or Medicare Part-C plan by Anthem Blue Cross and Blue Shield available to residents in Ohio.
Kaiser versus Anthem Blue Cross in California Anthem Blue Cross versus Kaiser - the Heavyweights of California. Local Anthem plans including Group IVR Medicare Supplemental plans such as Companion Plan 800 am. Anthem Enhanced Choice is an individual health plan that provides coverage for doctor visits prescriptions and more.
This plan includes additional Medicare prescription drug Part-D coverage. Pennsylvania Blue Shield. Learn more about limited duration insurance plans.
The benefits provided in this summary are subject to federal and. Available in select states there are six different plans and one may be right for you and your family. Hier sollte eine Beschreibung angezeigt werden diese Seite lässt dies jedoch nicht zu.
The PPO 40 plan does not cover the costs of cosmetic surgery or other surgical services related to beautification-including medical complications that arise from or are the result of cosmetic surgical procedures except for procedures related to reconstructive surgery to restore a deformity or correct a bodily function caused by injury or a medically necessary reconstructive surgical procedure. Anthem Link Balanced Blue Connection OAEPO 1000208000. - 500 pm Monday - Friday available 247 800832-6011 XVA XVB XVF XVG XVH XVI XVP Provider Service Individual Medicare Supplemental plans 800 am.
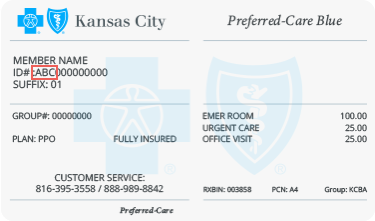
Contact HealthComp with member service eligibility. Blue cross blue shield plan code 040. If your plan includes out of network benefit and you use a non-network provider you are responsible for any difference between the covered expense and the actual non -participating providers charge.
Its always said that reading will always help you to overcome something to better. This plan includes additional Medicare prescription drug Part-D coverage. Employers Blue Cross Blue Shield Blue Distinction High-Performance Network Solutions.
WG Rx Group Number. 020099 Plan Code. Anthem Link Balanced Blue.
Blue Cross and Blue Shield of Oklahoma. The choice is yours. Anthem MediBlue Preferred HMO H3655-040 is a 2020 Medicare Advantage Plan or Medicare Part-C plan by Anthem Blue Cross and Blue Shield available to residents in Ohio.
Blue christmas clip art blue banner clipart blue border clipart blue t shirt clipart free blue ribbon clip art blue car clipart. Rather than enjoying a good PDF taking into account a cup of coffee in the afternoon instead they juggled past some harmful virus inside their computer. 6 an Pl Code 040 is a code used by Anthem Blue Cross to identify the USC plan.
The Anthem MediBlue Preferred HMO has a monthly premium of - and has an in-network Maximum Out-of-Pocket limit of 4900 MOOP. 20 coinsurance 40 coinsurance Primary care visit to treat an injury or illness 20 coinsurance 40 coinsurance Specialist care visit 20 coinsurance 40 coinsurance Pregnancy Maternity Care Physician office visit. 8 HealthComp is USCs Third Party Administrator TPA.
- 500 pm Monday - Friday IVR available 247. Anthem Link Balanced Blue Connection OAEPO 1000208000. Like the name says this type of plans deductible is higher than most traditional plans.
Even if you choose a plan that covers brand-name prescription drugs its still a good idea to consider using. Anthem blue cross ppo plan code 040 pyqdnx3 is friendly in our digital library an online admission to it. To qualify as an HDHP the IRS says a plan must have a deductible of at least 1350 for an individual.
Theres geographic flexibility so youre covered in many places and you may not always need a referral. Blue Cross and Blue Shield of Oregon. In-network preventive care is not subject to deductible if your plan has a deductible.
You may be asked for this number when contacting HealthComp. As youll see on the following pages some of our plans include Comprehensive drug coverage and some plans only include generics. The Anthem MediBlue Preferred HMO has a monthly premium of 0 and has an in-network Maximum Out-of-Pocket limit of 4200 MOOP.
WLHA IngenioRX is open 277 and can be reached at 833- 261-2463 Phone Number. 7 HealthComp Group Number is used by HealthComp to identify the USC account. Anthem Link Balanced Blue Connection OAEPO 2000205000.