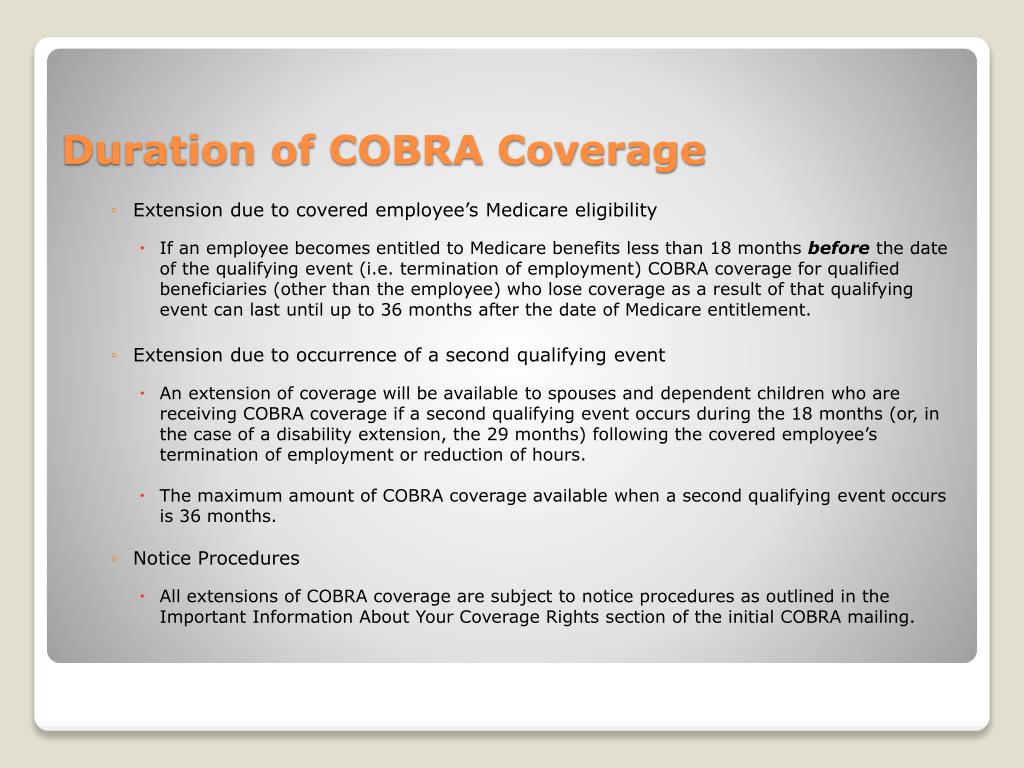
Although not the focus of this post the 18-month period may be extended to 29 months in the event of a disability and spouses and dependents have additional COBRA rights to elect up to 36 months of coverage due to certain other qualifying events including divorce or the employees death. If you are eligible to continue health coverage under federal COBRA for 18 months then you can continue coverage under state continuation coverage for an additional 18 months.
 What Is Cobra Bond Can You Elect Cobra After 60 Days
What Is Cobra Bond Can You Elect Cobra After 60 Days
What Happens After 18 Months On COBRA.
Cobra extension after 18 months. The provision does not extend your policys life beyond the normal 18 months though. What do I do when my COBRA runs out. There are other requirements that must be met as well.
However you may be eligible to convert your COBRA coverage to an individual policy from your insurance company if they offer an individual policy. The result is that extended COBRA coverage ends on the lat-er of the first day of the month that is more than 30 days after the determination or the initial 18-month period. The length of time depends on the type of qualifying event that gave rise to the COBRA rights.
The COBRA rules are complex. It suspends certain COBRA deadlines during the Outbreak Period starting from March 1 2020 and ending 60 days following the end of the COVID-19 national emergency. Generally this will include anyone who hador could have hadCOBRA as far back as November 2019 because their 18 months of coverage would extend through April 2021 she pointed out.
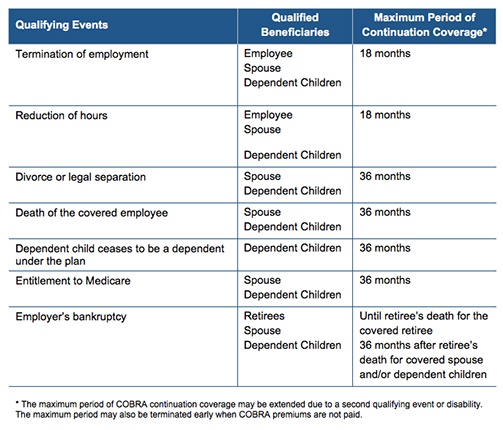
What if a qualified beneficiary is approved for the disability extension but later has a secondary event for. COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months. All qualified beneficiaries are generally eligible for continuation coverage for 36 months after the date the qualified beneficiarys benefits would otherwise have terminated.
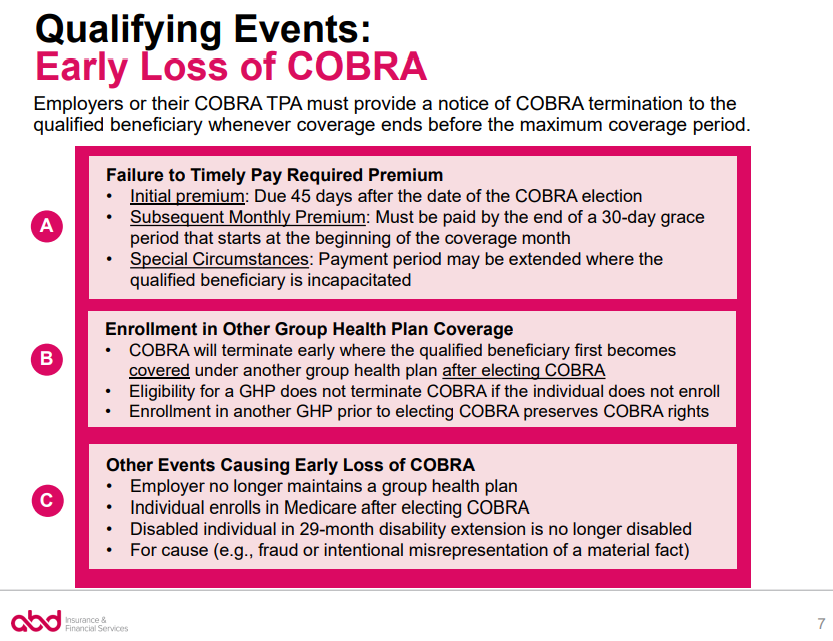
Keep in mind if you choose to terminate your COBRA continuation coverage early with. COBRA coverage can be extended from 18 to 29 months if the qualifying event is the employees termination quitting or reduction in hours and the beneficiary either has a disability at the time of the qualifying event or becomes disabled during the first 60 days of COBRA coverage. For more information on COBRA.
The second is when a second qualifying event occurs. To exhaust COBRA continuation coverage you or your dependent must receive the maximum period of continuation coverage available without early termination. The first is when a qualified beneficiary is disabled.
If you are entitled to an 18 month maximum period of continuation coverage you may become eligible for an extension of the maximum time period in two circumstances. A plan however may provide longer periods of coverage beyond the maximum period required by law. You have up to a total of 36 months of coverage when combining the.
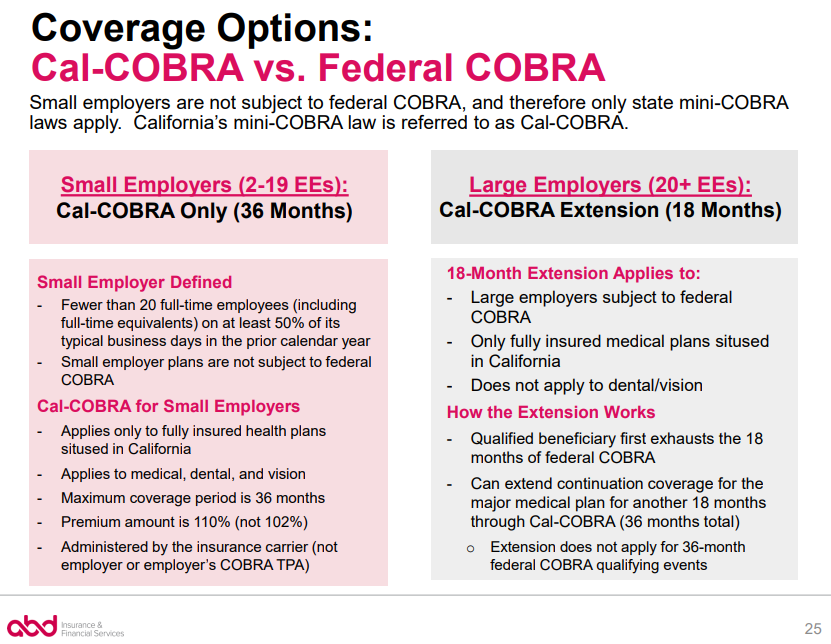
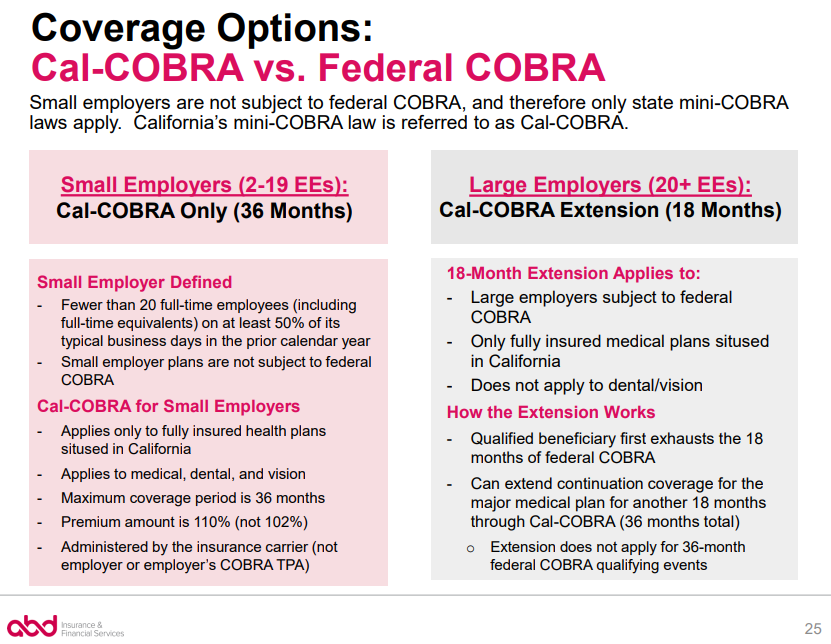
Unfortunately you can not remain on COBRA unless there is a new qualifying event. Since the Affordable Care Act running out of COBRA continuation coverage is now a qualifying life event which means that you now have a special enrollment period in which you may enroll in an insurance plan outside of open enrollment. Can I get Cal-COBRA if I had Federal COBRA.
In California if your employer has two to 19 employees you may be covered by Cal-COBRA. When Federal COBRA ends eligible employees can buy 18 months additional health coverage under Cal-COBRA. Within 30 days after the date of that determination.
Cal-COBRA may also be. In addition the extended period of COBRA ends if there is a final determination under. You have 30 days from the termination date of COBRA coverage to request this individual policy.
Can I extend my COBRA continuation coverage. An employer may extend the maximum COBRA continuation coverage period beyond the 18 or 36 months required by law. The IRS and DOL have released a final rule that extends certain deadlines for COBRA continuation coverage.
Finally the covered employee must generally notify the plan administrator about the disability determination within 60 days after the date the disability determination is issued but in no case later than the end of the 18-month period of continuation coverage that applies to the qualifying event. The employer should specify in the COBRA policy when coverage will be extended. While the bankruptcy rule is not an extending rule it is included in this guide because it results in longer coverage than the average 18 or 36 months.
COBRA you wont be eligible for special enrollment in another group health plan such as a spouses plan until you have a new special enrollment event such as marriage birth of a child or if you exhaust all COBRA coverage available to you COBRA coverage typically lasts 18 months but may last longer in certain circumstances.
 Ppt Cobra Continuation Coverage Powerpoint Presentation Free Download Id 775915
Ppt Cobra Continuation Coverage Powerpoint Presentation Free Download Id 775915
 Frequently Asked Questions New York State Cobra Extension Pdf Free Download
Frequently Asked Questions New York State Cobra Extension Pdf Free Download
Cobra Extensions And Medicare Csnw Benefits
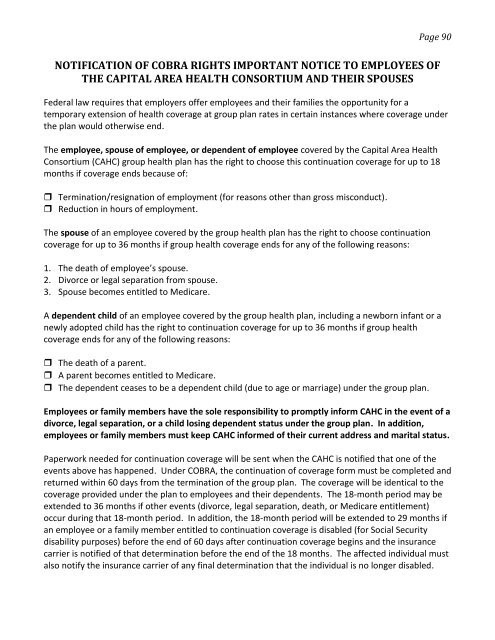 Notification Of Cobra Rights Important Notice To Employees Of The
Notification Of Cobra Rights Important Notice To Employees Of The
 What Qualifying Events Trigger Cobra
What Qualifying Events Trigger Cobra
 Cobra Initial Notice Template Bsi Does Not Administer
Cobra Initial Notice Template Bsi Does Not Administer
 Model Cobra Continuation Coverage General Notice
Model Cobra Continuation Coverage General Notice
 Early Termination Of Cobra Upon Enrollment In Other Group Health Plan Or Medicare Abd Insurance Financial Services
Early Termination Of Cobra Upon Enrollment In Other Group Health Plan Or Medicare Abd Insurance Financial Services
Https Www Bcbstx Com Pdf Forms Grp Cobra Continuation Tx Pdf
![]() How Long Does Cobra Last The Answer It Depends Basic
How Long Does Cobra Last The Answer It Depends Basic
 Cobra Small Employer Exception Abd Insurance Financial Services
Cobra Small Employer Exception Abd Insurance Financial Services
Https Silo Tips Download Frequently Asked Questions New York State Cobra Extension

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.