Medical services PDF. Washington - 1 800 206-1244.

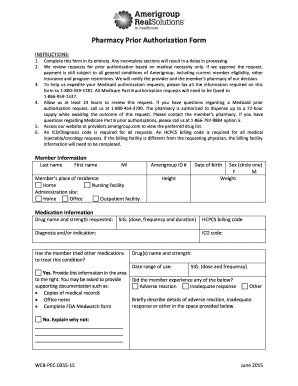
Required on some medications before your drug will be covered.
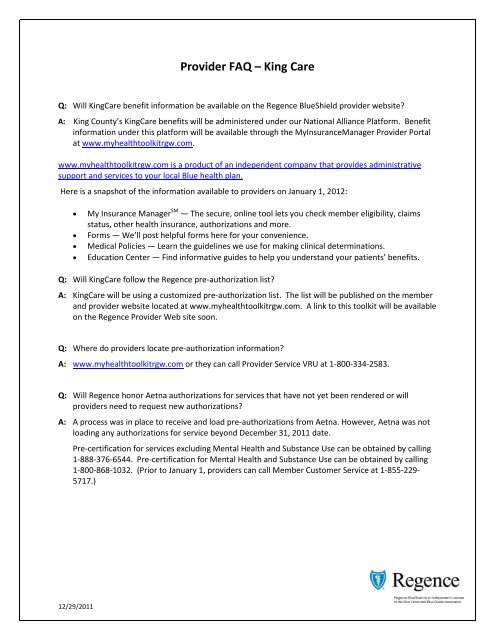
Regence prior authorization phone number. Please provide a detailed description of the service for preauthorization to a member of our Customer Care Team at 1-866-738-3924 and they will let you know if the service requires preauthorization. Ordering care providers will complete the notificationprior authorization process online or over the phone. Easily obtain pre-authorization and eligibility information with our tools.
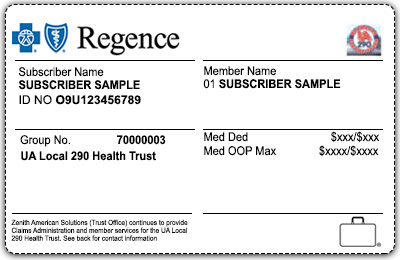
How do I determine if a diagnosis or procedure code needs preauthorization. Regence BlueShield serves select counties in the state of Washington and is an Independent Licensee of the Blue Cross and Blue Shield Association. 1 2017 notification is required for certain genetic and molecular lab tests for certain UnitedHealthcare Commercial benefit plans.
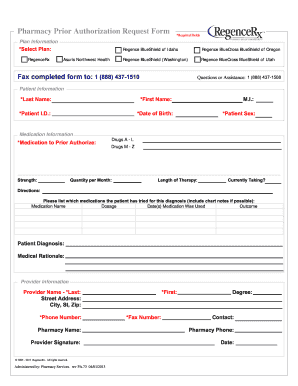
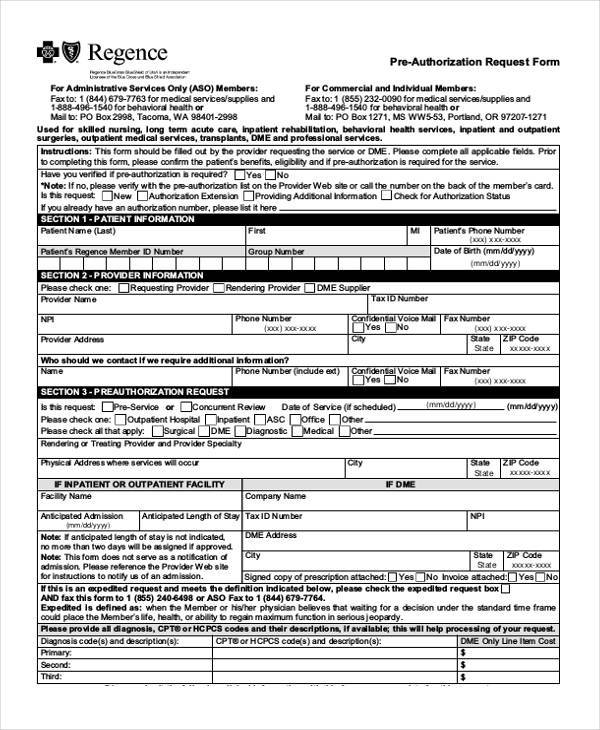
Providers submit an electronic pre-authorization request through the Availity Portal via a pre-authorization request form through the AIM Specialty Health Portal or the eviCore portal. 1 877 663-7526 or. Diagnosis codes and descriptions.
Labs must register their tests to participate as part of the Genetic and Molecular Lab Testing NotificationPrior Authorization process. For providers to obtain prior authorization Medica requires that the following information be provided. Monday through Friday 6 am.
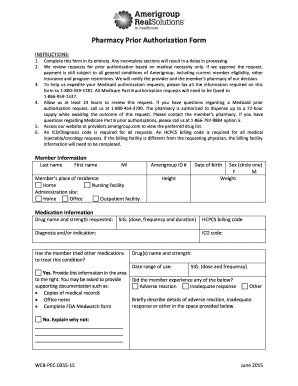
Prior to completing this form please confirm the patients benefits eligibility and if pre-authorization is required for the service. We are unable to quote a benefit by a diagnosis or procedure code. CPT or HCPCS codes and descriptions.
Regence BlueShield serves select counties in the state of Washington and is an Independent Licensee of the Blue Cross and Blue Shield Association. Refer to the Important Pre-authorization Reminders section for details. To 800 pm Monday through Friday from October 1 through February 14 our telephone hours are 800 am.
Utah - 1 800 782-8211. Oregon - 1 800 448-0525. Submit the appropriate pre-authorization request form only if unable to submit online or if submitting an expedited request.
To 800 pm seven days a week. PT Idaho - 1 888 526-5321. It is quicker than calling and allows you to easily view and print your assigned order number.
TransactRx and CoverMyMeds are separate and independent companies that provide pharmacy pre-authorization and claims submission for Regence members. We are the service-oriented partner employers trust. Our team of caring experts design and deliver high-quality innovative and affordable health plans for self-funded employers.
Parkland Community Health Plan will notify the requesting provider and member by a phone call and in writing of missing information no later than three 3 business days after the prior authorization receive date. Name and phone number of the provider who is making the request. TTY users should call 711.
If the request is not approved please remember that you always have the option to purchase the medication at your own expense. Prior authorization is required for selected services. If your health plans formulary guide indicates that you need a Prior Authorization for a specific drug your physician must submit a prior authorization request form to the health plan for approval.
2021 Regence BlueShield. Other Blue Plans pre-authorization requirements may differ from ours. Phone or fax.
To verify coverage or benefits or determine pre-certification or pre-authorization requirements for a particular member call 1-800-676-BLUE or send an electronic inquiry through your established connection with your local Blue Plan. To determine if pre-authorization is required please use the electronic authorization tool on the Availity Provider Portal review our pre-authorization lists or call the phone number on the back of the members card. View pharmacy pre-authorization requirements and medication policy and submit pre-authorization requests using CoverMyMeds.
Regence BlueShield is an HMO plan with a Medicare contract. Contact AIMs call center at 1 877 291-0509 to submit order number requests. National BlueCard member benefits and eligibility.
DME Only Line Item Cost For Uniform Medical Plan UMP Members. An incomplete prior authorization PA request is a request for a service that is missing information needed to decide medical necessity. 18884270470 toll free Mon-Fri 700 am.
Phone 1 800 676-2583 Monday through Friday 730 am. Name phone number address and type of specialty of the provider to whom the patient.
Https Www Pathway Com Wp Content Uploads 2017 06 Regence Bs Of Or Wa Prior Auth Form Pdf
 Provider Faq King Care Regence Blueshield
Provider Faq King Care Regence Blueshield
 Blue Coverage For Regence Healthwise Members Will Not Terminate Blue Cross And Blue Shield Of Texas
Blue Coverage For Regence Healthwise Members Will Not Terminate Blue Cross And Blue Shield Of Texas
 Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
 R E G E N C E P A F O R M Zonealarm Results
R E G E N C E P A F O R M Zonealarm Results
 Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Https Www Primetherapeutics Com Content Dam Corporate Documents Resources Pharmacists Processingresources Planannouncements Document Planannouncement Regencehealthplans Asuris Bridgespan Pdf
Https Www Regence Com Documents 10192 4153375 Prescription Coverage Determination A842eb00 7c07 4429 B8cf E698d7650f3a
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
 Blue Coverage For Regence Healthwise Members Will Not Terminate Blue Cross And Blue Shield Of Texas
Blue Coverage For Regence Healthwise Members Will Not Terminate Blue Cross And Blue Shield Of Texas
Https Beonbrand Getbynder Com M 6cc14125643a10d3 Original Pre Authorization Request Form Or Pdf
 Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
 Fillable Online 2017 Regence Bluecross Blueshield Of Utah Pre Authorization Request Form 2017 Regence Bluecross Blueshield Of Utah Pre Authorization Request Form Fax Email Print Pdffiller
Fillable Online 2017 Regence Bluecross Blueshield Of Utah Pre Authorization Request Form 2017 Regence Bluecross Blueshield Of Utah Pre Authorization Request Form Fax Email Print Pdffiller

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.