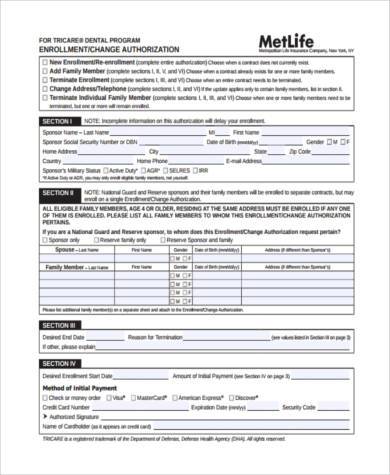
To be used only for prescriptions which are to be filled through the Department of Defense DoD TRICARE pharmacy program TPHARM. Check to see if we offer a Letter of Attestation you can attach instead of clinical documentation.
 Tricare Formulary Fill Online Printable Fillable Blank Pdffiller
Tricare Formulary Fill Online Printable Fillable Blank Pdffiller
You dont need to send multiple forms.
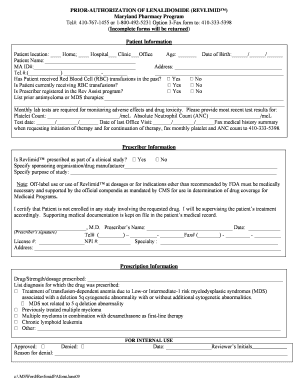
Tricare medication prior authorization form. Brand over Generic Prior Authorization Request Form To be completed and signed by the prescriber. All Other Beneficiaries Enrolled in a TRICARE Prime Plan. Prior authorizations for certain services andor procedures require Health Net Federal Services LLC HNFS review and approval prior to being provided.
You must have prior authorization for all specialty care. Please complete the form and submit it to Humana by following the instructions on the form. The patient may attach the completed form to the prescription and mail it to.
Your provider can either call the Express-Scripts prior authorization line 1-866-684-4488 or heshe can fill out the prior auth form that is linked to that medication on the. Smoking cessation programs. Prior authorization is not required for injection infusion medication when it is provided in a providers office or other outpatient setting unless the beneficiary is an active duty service member.
Kentucky Medicaid Authorization Form. Please complete patient and physician information please print. Simply select the beneficiarys TRICARE plan option for example TRICARE Prime or TRICARE Prime Remote the beneficiary.
Concurrent hospice and curative care monthly service activity log. A TRICARE prior authorization form is a document to be completed by a prescribing physician requesting a specific type of medication for their patient which is otherwise not covered by their TRICARE plan. Express Scripts PO Box 52150 Phoenix AZ 85072- 9954 or email the form only to.
Find TRICARE claims forms our medical questionnaire and other important documents all collected in one convenient place. Give the form to your provider to complete and send back to Express Scripts. Prescription drug prior authorization request form PDF opens new window.
TRICARE doesnt cover drugs that arent medically or psychologically necessary for the diagnosis or treatment of a covered illness. If youre enrolled in a TRICARE Prime plan your primary care manager PCM will work with your regional contractor for the prior authorization. Check if we offer a Letter of Attestation you can attach instead of clinical documentation.
You can call or register on your contractors site for secure services. Non-network providers are encouraged to submit online as electronic requests save time and improve accuracy. The Service Code entered is for.
Download and print the form for your drug. This will expedite the review process. Youll get an authorization.
Use our Prior Authorization Referral and Benefit tool. Prior Authorization Forms. Our electronic prior authorization ePA solution is HIPAA-compliant and available for all plans and all medications at no cost to providers and their staff.
Search for your drug on the TRICARE Formulary Search Tool. You must have prior authorization for all specialty care. Inpatient TRICARE Service RequestNotification Form Network providers requesting prior authorization for an elective admission or submitting an inpatient admission notification are required to submit online.
Important message from TRICARE. Is it a limited benefit. You need to contact your regional contractor for prior authorization.
You also need a fitness-for-duty review for. Tricares Preferred Method for Prior Authorization Requests CoverMyMeds is the fastest and easiest way to review complete and track PA requests. Prior Authorization Referral Benefit Tool.
Physicians and health care practitioners in Kentucky may use this form to submit authorization requests for their Humana-Medicaid covered patients. Avoid extra work and first check if HNFS approval is needed. Laboratory Developed Tests LDT attestation form.
Your primary care manager gets your referral and prior authorization. Instructions are on the form. Learn about TRICAREs Prescription Drug Coverage Find Medical Necessity and Prior Authorization Forms.
The provider may call. Express Scripts is the TPHARM contractor for DoD. The Prior Authorization Referral and Benefit Tool allows you to easily determine if an approval from Health Net Federal Services LLC HNFS is required.
Have you checked requirements. TRICARE is a civilian health care program for military personnel and their dependents therefore the Department of Defense D0D only authorizes drug therapy for patients if it is the most effective. Requesting Prior Authorization.
Continuous glucose monitor attestation form. We make it easy to share information Get your written prescriptions to us by using our mail order form. Prior authorization is required for home infusion for all beneficiaries.
Your authorization approval will apply to network pharmacies and home delivery.






