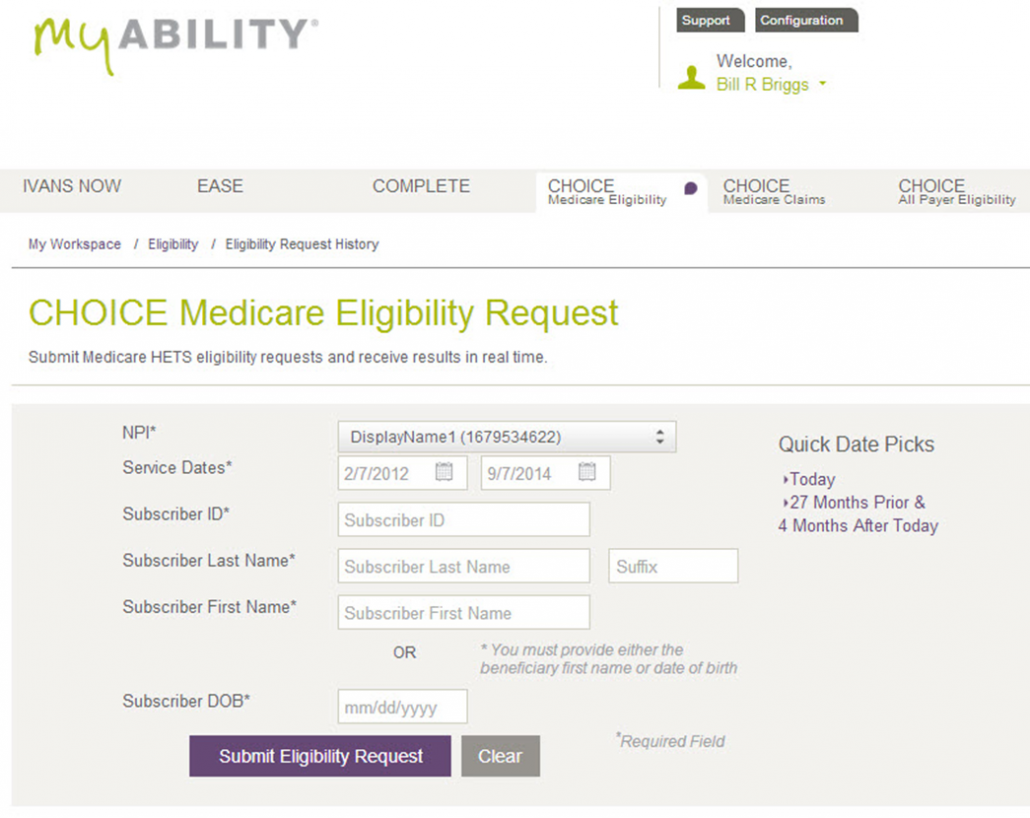
Billing agencies clearinghouses or software vendors can also verify Medicare coverage. Using an eligibility and benefits report can benefit the health of your practice and your patients.
Https Www Cms Gov Files Document Checking Medicare Eligibility Print Friendly Pdf
Submit a HIPAA 270 transaction eligibility to BCBSND.
Verify medicare eligibility and benefits for providers. A Simple Eligibility and Benefits Phone Call Script Time to get on the phone and call up your favorite insurance company to verify coverage for your new patient. Information Needed to Check Medicare Eligibility. You may also verify eligibility by calling.
Please enter required fields to verify eligibility. The following script will help you hit all the major points but also realize most insurance reps will. Some questions may involve the work history of the spouse or partner to see if one or both may be eligible for Social Security benefits and Medicare.
The following provides information about the systems available to CGS home health and hospice providers to check a beneficiarys eligibility. You need to identify coverage fast and reduce the number of claims being denied on the back end due to inactive insurance or non-coverage. There are many things that can influence the patients responsibility such as whether or not the.
Inquire on eligibility and benefits electronically simply click on the plans associated website to learn how to get eligibility and benefits information for your patients in that plan. Get a copy of the digital ID card. HETS transactions require system capabilities that some providers prefer to contract out to a third-party entity.
Systems for Checking Medicare Eligibility. Go to the Eligibility tab on the Main Menu. Date of birth month day and 4-digit year Gender.
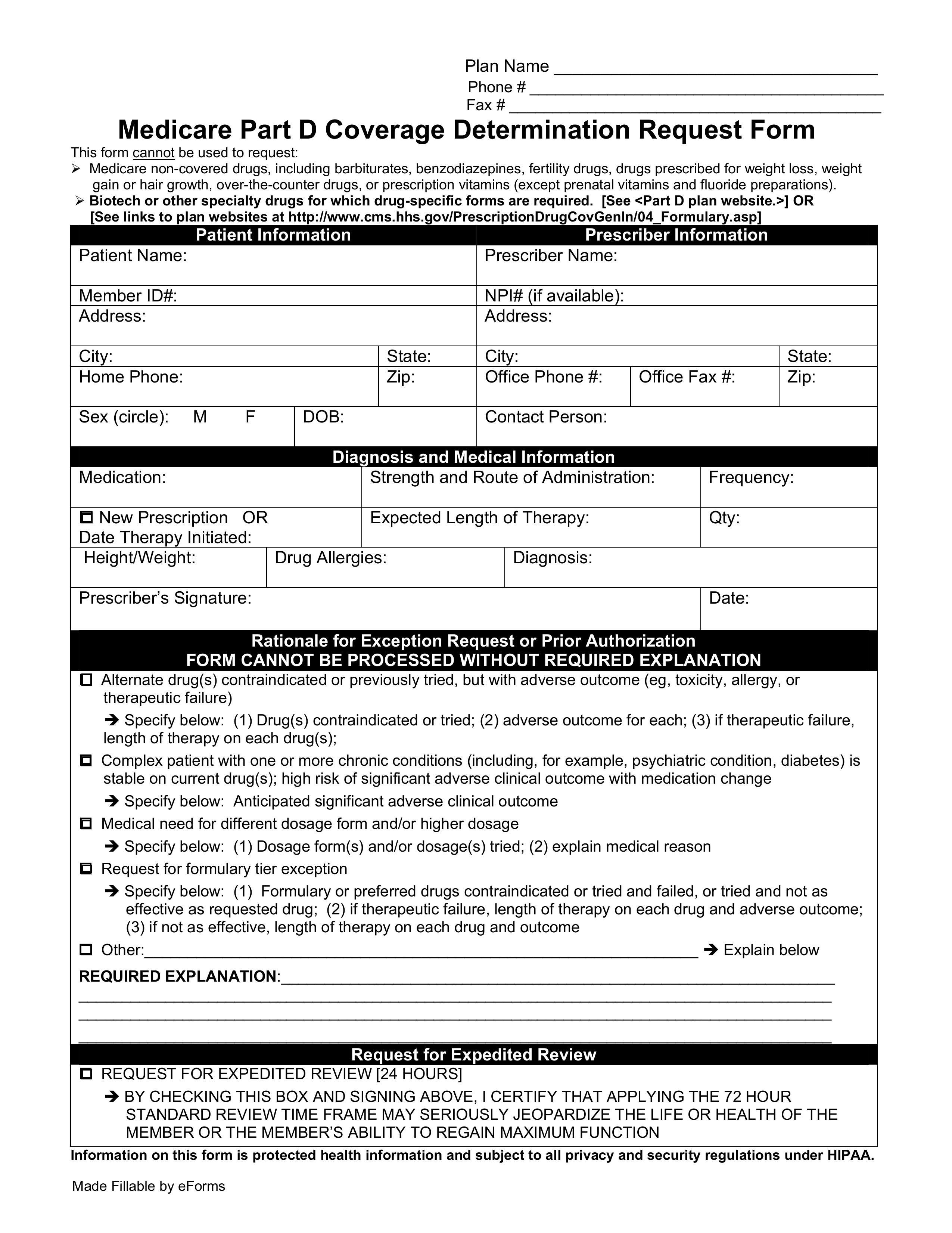
CVS Caremark Pharmacist Help Desk at 1-800-364-6331 Part D CVS Caremark Pharmacist Help Desk at 1-866-693-4620. Eligibility and Benefits MedCost. One must provide identification and this includes a full name address date of birth and Social Security number.
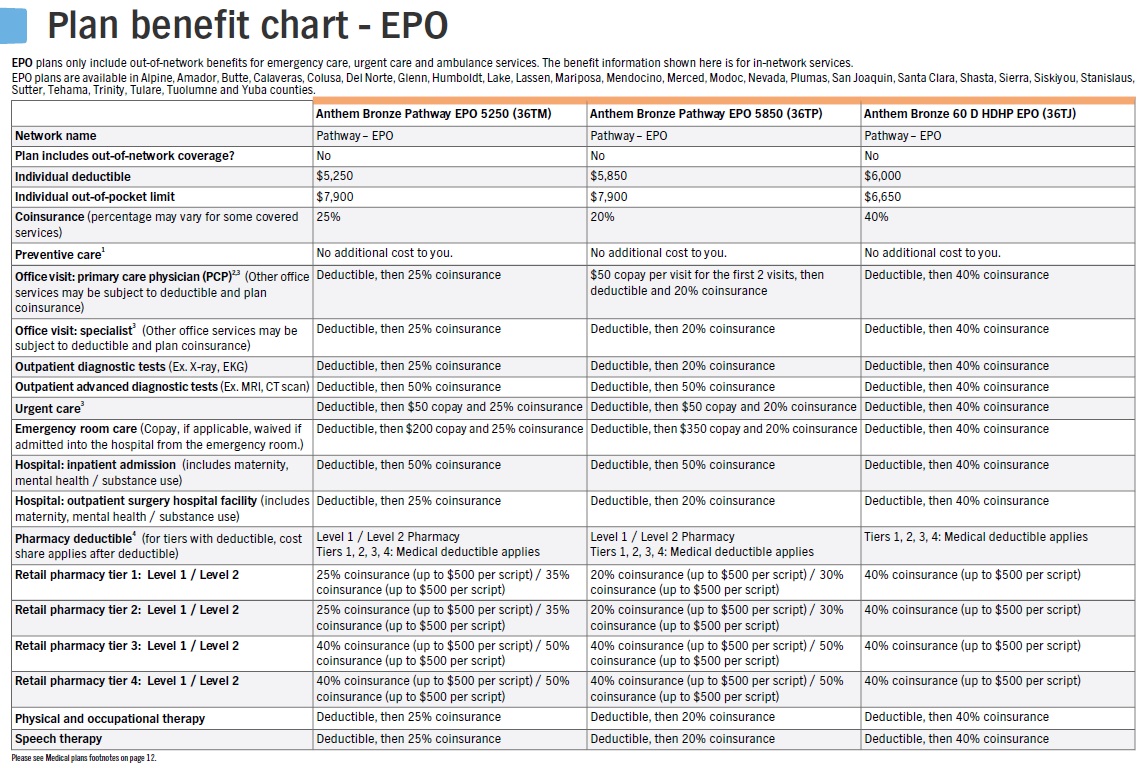
Check coverage limits and therapy accumulators. Eligibility and benefits verification can be complex with patients taking on more payment responsibility and frequently changing insurance providers. Learn more about our Eligibility and Benefits tool.
Many providers use the eligibility data ahead of appointments to verify the Medicare beneficiary is eligible for the service scheduled. Under Benefits select Schedule of Benefits link to locate specific member benefits information. The First and Last name must match the beneficiarys Medicare card.
Send an electronic inquiry through the Availity Provider Portal. CWF verifies the beneficiarys entitlement to Medicare deductible status available benefits. Aetna Health and Life Insurance Company.
First and last name. Verify the care providers network and tier status for the members plan. Its easy to verify eligibility and find out about the members benefits.
Verify eligibility and benefits using one of three methods. Example if you use a billing agent to submit claims the billing agent can also verify Medicare. For information on how providers can verify member eligibilty refer to the Providers chapter of the Tufts Health Public Plans Provider Manual.
Eligibility and benefit tips. View cost share amounts and balances. Out-of-state BlueCard plans and out-of-state.
PVerifys Eligibility integrations automate patient extraction for a specific DOS to verify in advances and returns the benefits directly into the integrated system most often as a patient note In addition to the inserted data pVerify offers the First-Class Batch Excel Report for easy filtering and patient review. Use our Eligibility and Benefits tool to. Enter the required Beneficiary Details fields.
Medica Member eligibility will be verified through the CVS Caremark claim processing system. Provide at least one of the following. The HIPAA Eligibility Transaction System HETS is intended to allow the release of eligibility data to Medicare Providers Suppliers or their authorized billing agents for the purpose of preparing an accurate Medicare claim determining Beneficiary liability or determining eligibility for specific services.
Common Working File CWF is a system that contains all Medicare beneficiary information as well as claim transactions which includes Medicare Part A Part B and Durable Medical Equipment. The Fiscal Intermediary Standard System and Multi-Carrier System processing systems interface with CWF to process claims. Secure Provider Portal Log in to verify member eligibility.
To check Medicare eligibility you must have the following beneficiary information. Where you cant. Aetna Life Insurance Company.
Search benefits by category including vision. You can see plans and associated payer IDs to look up eligibility and benefits information electronically. Call the BlueCard Eligibility line at 800-676-BLUE 2573 and provide the prefix.
American Continental Insurance Company of Brentwood Tennessee.